Poster Session
Rheumatoid Arthritis (RA)
Poster Session A
Session: (0430–0469) Rheumatoid Arthritis – Diagnosis, Manifestations, and Outcomes Poster I
0433: In-hospital outcomes of patients admitted due to First-Time Pulmonary Embolism with preexisting Rheumatoid Arthritis: A Nationwide Analysis 2016-2022
Sunday, October 26, 2025
10:30 AM - 12:30 PM Central Time
Location: Hall F1
.jpg)
Hospitalization Rates of patients admitted for First Time PE with preexisting RA steadily increased from 2016 to 2022.
.jpg)
The majority of inpatients were White followed by Black and Hispanic individuals.
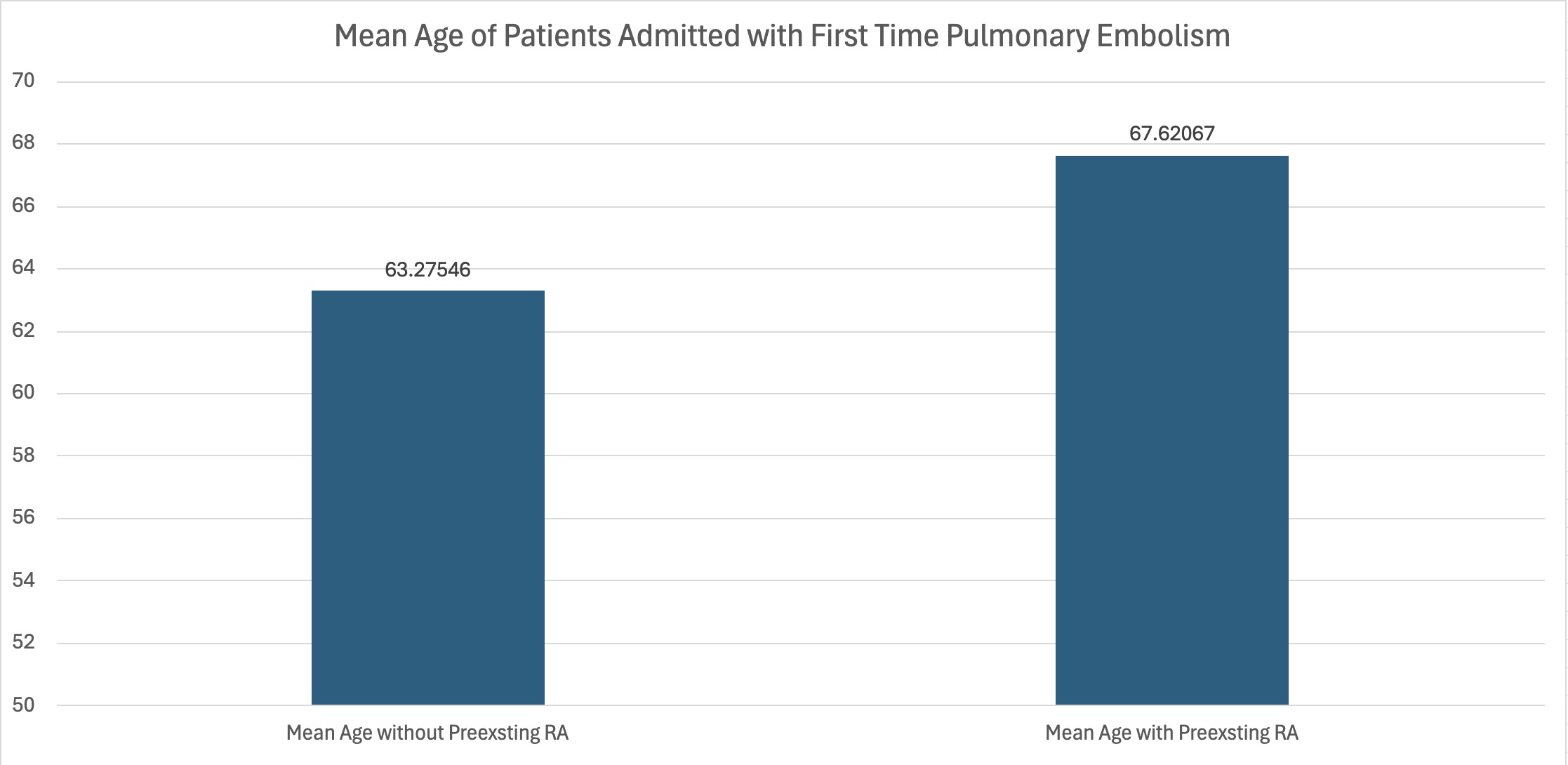
Individuals without preexisting RA were hospitalized at earlier ages.
- KB
Karuna Bista, MD (she/her/hers)
Montefiore New Rochelle Hospital
New Rochelle, New York, United StatesDisclosure(s): No financial relationships with ineligible companies to disclose
Abstract Poster Presenter(s)
Background/Purpose: Although it has been documented that patients with Rheumatoid Arthritis may be at increased risk of Pulmonary Embolism, other inpatient outcomes remain largely unexplored. We aimed to better identify the impact of Rheumatoid Arthritis on hospital outcomes in patients admitted for first-time Pulmonary Embolism.
Methods: A retrospective cohort analysis using the U.S. HCUP NIS Database from 2016-2022 was conducted. Patients admitted with a primary diagnosis of a first episode of Pulmonary Embolism with preexisting Rheumatoid Arthritis were identified using ICD-10 codes. The primary outcome was in-hospital mortality. Secondary outcomes were length of stay, resource utilization and need of various interventions. Univariate analysis was done and variables with p< 0.2 were considered for multivariate analysis, adjusting by age, gender, race, Charlson comorbidity index, hospital location and teaching status, size, region and insurance status. Data was considered statistically significant with p-value < 0.05.
Results: From 2016 to 2022, a total of 1,315,394 patients were admitted for a first-time pulmonary embolism (PE). Out of these, 30,474 patients, or 2.32%, had a preexisting diagnosis of rheumatoid arthritis (RA). Notably, these RA patients demonstrated a 35.19% reduction in the odds of mortality (p-value = 0.00). Additionally, they experienced an average decrease in the length of hospital stay by 0.3764 days (p-value = 0.001) and a significant reduction in mean total charges for their hospital stay, amounting to $6,886.12 (p-value = 0.00). Furthermore, RA patients had a 27.87% lower likelihood of undergoing intubation during their hospitalization (p-value = 0.001).
Conclusion: Our research revealed that Rheumatoid Arthritis is associated with improved inpatient outcomes with patients with first-time Pulmonary Embolism. These findings suggest that Rheumatoid Arthritis may confer a protective effect in this population, warranting further investigation.

