Poster Session
Metabolic Bone Disease
Poster Session C
Session: (2106–2123) Osteoporosis & Metabolic Bone Disease – Basic & Clinical Science Poster II
2107: Experience of a Fragility Fracture Coordination Unit Integrated Across Two Hospitals: An Innovative Multidisciplinary Model for Optimizing the Management of Geriatric and Non-Geriatric Patients Beyond Surgery After an Osteoporotic Bone Fragility Fracture
Tuesday, October 28, 2025
10:30 AM - 12:30 PM Central Time
Location: Hall F1
- CE
César Antonio Egües Dubuc, MD,MSc (he/him/his)
Hospital Universitario Donostia
San Sebastian, SpainDisclosure(s): No financial relationships with ineligible companies to disclose
Abstract Poster Presenter(s)
Background/Purpose: Fracture Coordination Units typically function within a single hospital using a multidisciplinary approach. Our unit, established in February 2024, pioneers a model coordinating care between two hospitals: University Hospital of Donostia (UHD) and Matía Hospital (MH). It integrates Rheumatology (REU), Internal Medicine (I.M.), and Traumatology at UHD, alongside Orthogeriatrics (OG) at MH, ensuring a patient-centered approach. Patients at UHD are assessed by I.M.; those with a geriatric profile transfer to MH for OG management, while others receive osteoporotic treatment from REU at UHD. After over a year of operation, evaluating clinical differences and therapeutic approaches between REU and OG group to understanding the impact of multidisciplinary coordination on patient care and osteoporosis treatment.
Methods: This study analyzes the clinical differences and management of patients treated by REU and OG between February 1, 2024, and April 15, 2025, using a cross-sectional descriptive design. Clinical, analytical, and treatment variables were collected, with statistical analyses performed in SPSS. Categorical variables were expressed as frequencies and percentages, continuous variables were presented as medians with confidence intervals. Chi-square and Mann-Whitney U tests assessed associations. Missing data were handled through regression-based imputation to ensure result integrity.
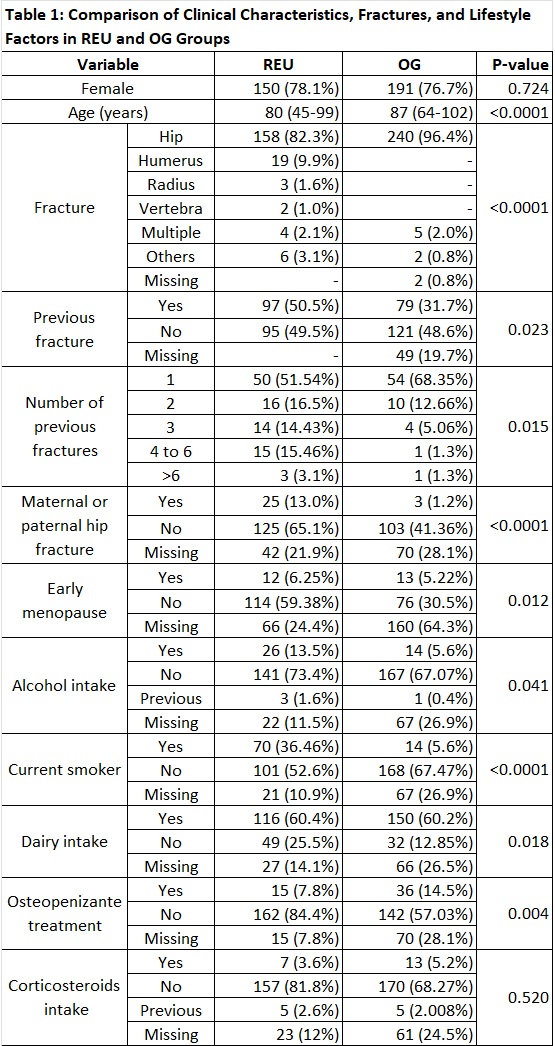
Results: Significant differences were observed between the RHE (n=192) and OG (n=249) groups. OG were older (87 vs. 80 years; p< 0.0001), and hip fractures were more prevalent (96.4% vs. 82.3%; p< 0.0001). Risk factors were more common in RHE, including early menopause (p=0.012), family history of hip fracture (p< 0.0001), smoking (p< 0.0001), and alcohol consumption (p=0.041). Previous fractures were more frequent in RHE (50.5% vs. 31.7%; p=0.023), with greater variability in fracture count (Table 1).
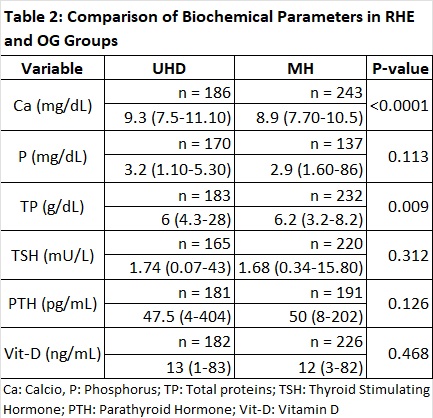
Biochemically, RHE showed higher serum calcium levels (9.3 mg/dL vs. 8.9 mg/dL; p< 0.0001), while OG had slightly higher total protein levels (6.2 g/dL vs. 6 g/dL; p=0.009) (Table 2).
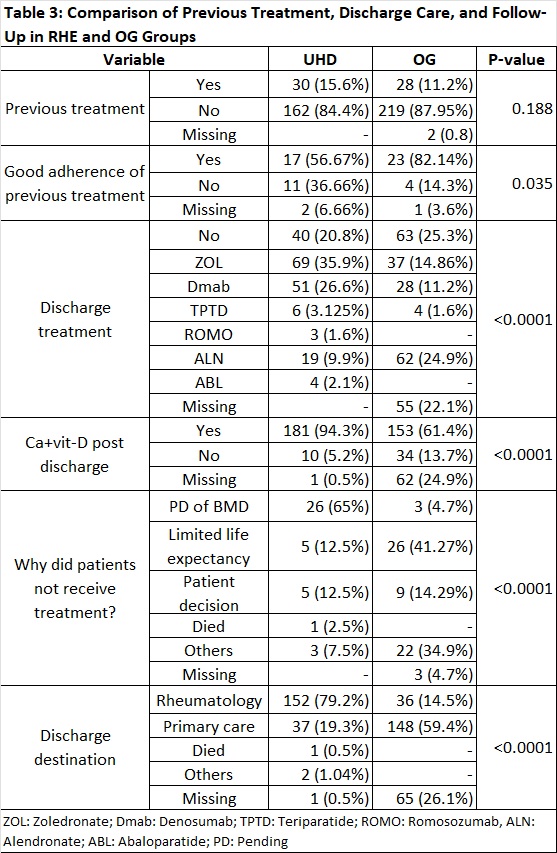
Discharge treatment, RHE patients received higher rates of calcium and vitamin D supplementation (94.3% vs. 61.4%; p< 0.0001) and osteoporosis therapy (79.2%; p< 0.0001). Zoledronate and denosumab were more commonly prescribed in RHE, while alendronate was the predominant treatment in OG. Reasons for lack of treatment differed between groups: in RHE, the primary reason was pending bone mineral density (BMD) evaluation before initiating therapy (65% vs. 4.7%; p< 0.0001). In OG, limited life expectancy was the most cited reason (41.27%) (Table 3).
Conclusion: These findings highlight distinct management approaches: REU follows a structured osteoporosis treatment strategy, while OG prioritizes patient stability. Higher fracture prevalence in REU correlates with greater risk factors, and rheumatologists tend to be more precise in fracture identification than geriatricians. A multidisciplinary approach is essential for optimizing osteoporosis care and tailoring treatments effectively.

