Poster Session
Scleroderma
Poster Session B
Session: (1553–1591) Systemic Sclerosis & Related Disorders – Clinical Poster II
1588: Prevalence Of Oral Manifestations And Their Association With Clinical And Serological Profile In Systemic Sclerosis Patients- An Indian Study
Monday, October 27, 2025
10:30 AM - 12:30 PM Central Time
Location: Hall F1
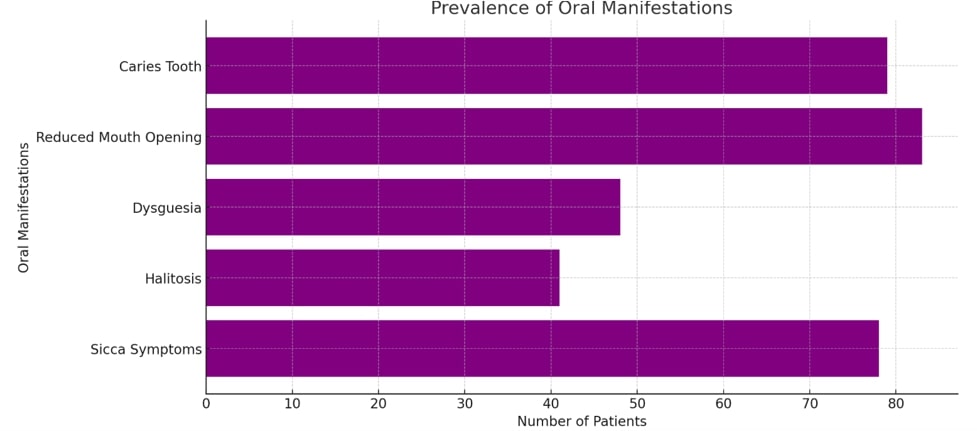
Prevalence Of Oral Manifestations In Systemic Sclerosis Patients
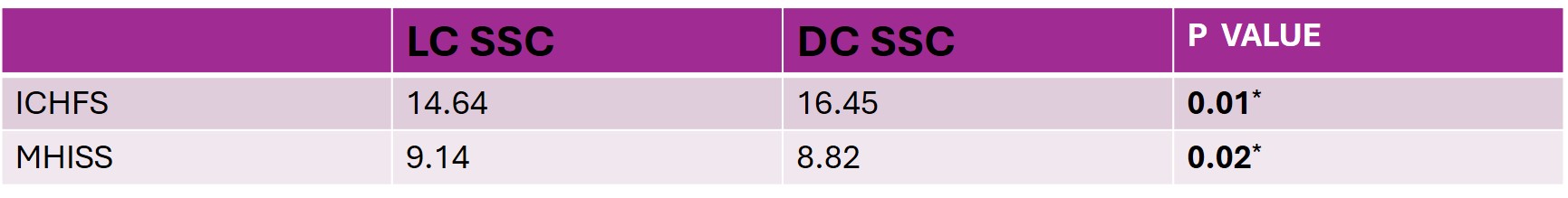
Functional Measures Among Limited and Diffuse Cutaneous Systemic Sclerosis Patients
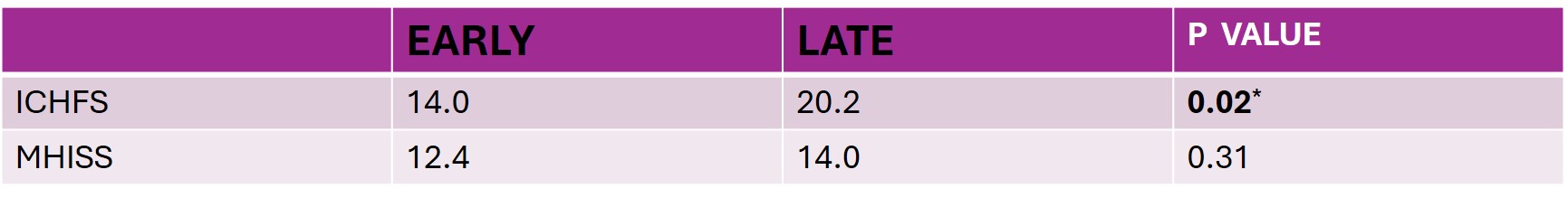
Functional Measures Among Early and Late Systemic Sclerosis Patients
- TR
Tejaswini Ramineni, n/a (she/her/hers)
Esic Medical College And Hospital, Sanathnagar
Hyderabad, Telangana, IndiaDisclosure information not submitted.
Abstract Poster Presenter(s)
Background/Purpose: Systemic sclerosis (SSC) is a chronic, multisystem autoimmune disease characterized by immune dysfunction, microangiopathy, and tissue remodelling. Orofacial manifestations, including xerostomia, microstomia, tooth decay, and periodontitis, affect up to 80% of SSC patients and significantly impact their quality of life. Despite their prevalence, these manifestations are often neglected compared to more life-threatening complications such as lung or kidney involvement. This study was designed to estimate the prevalence of oral-manifestations and to find their association with clinical and serological profiles in SSC patients.
Methods: A multi-centre study was conducted involving 131 SSC patients fulfilling ACR/EULAR-criteria. Comprehensive clinical-evaluation was performed including Modified-Rodnan-Skin-Score (MRSS) for skin tightness and Medsger’s-disease-severity-score for organ involvement. Oral-manifestations like presence of sicca symptoms, GERD were noted. Standardised-questionnaires like, Indian Cochin hand function Scale (ICHFS), Mouth Handicap in Systemic Sclerosis Scale (MHISS) were used to assess functional-impairment. Oro-facial health was evaluated using standardized dental indices such as Debri-Index(DI), Calculus-index(CI), number of missing-teeth, tooth-mobility, probing-depth(PD), gingival-bleeding(GB) and Clinical-attachment-level(CAL), Recession(REC) by a periodontist. Statistical-analysis was conducted using SPSS software V20, with statistical significance set at p < 0.05.
Results: Among 131 SSC patients, 45 were Limited Cutaneous SSC (LCSSC), 83 were Diffuse Cutaneous SSC (DCSSC) and 3 were sine scleroderma. The mean age was 42 years. Prevalence of oral manifestations like sicca symptoms was 59.5%, halitosis was 31.3%, Dysguesia was 36.6%, Reduced mouth opening was 63.4%, caries tooth was 60.3%%. Most of the oral manifestations were seen with a higher prevalence in DCSSC. Among the dental-examination findings, GB20,30,40, mean CAL, mean REC, DI and CI were higher in DSCC. The patients with early-disease ( < 5 years from first non-Raynauds symptom) constituted 43.5% and late-disease constituted 56.5%. All the oral-manifestations and dental-examination findings were higher in patients with late disease. The IC-HFS is higher in DCSSC patients with a mean score of 16.45 (p < 0.05) and among those with late disease with a mean score of 20.2(p < 0.05). Disease severity assessed by Medsger's score correlated positively with DCSSC, periodonditis, missing teeth, teeth mobility, GB, mean REC.
Conclusion: In this multicentre study, DCSSC exhibited significantly higher oral and dental manifestations with increased IC-HFS scores, GERD, reduced mouth opening, greater number of missing-teeth and periodontitis. Patients with late disease had more pronounced oral-manifestations and higher CAL, REC scores. These findings suggest that DCSSC and extended disease-duration are associated with more severe oral health complications, highlighting the importance of early dental intervention. Disease severity as assessed by Medsgers-score correlated-positively with presence of periodontitis indicating its possible role in disease pathogenesis.

