Poster Session
Epidemiology, Health Policy, and Outcomes
Poster Session C
Session: (1877–1913) Epidemiology & Public Health Poster III
1883: Temporal Patterns of Cardiometabolic Comorbidities Before and After Psoriatic Arthritis Diagnosis: A Nationwide Retrospective Study from Poland.
Tuesday, October 28, 2025
10:30 AM - 12:30 PM Central Time
Location: Hall F1
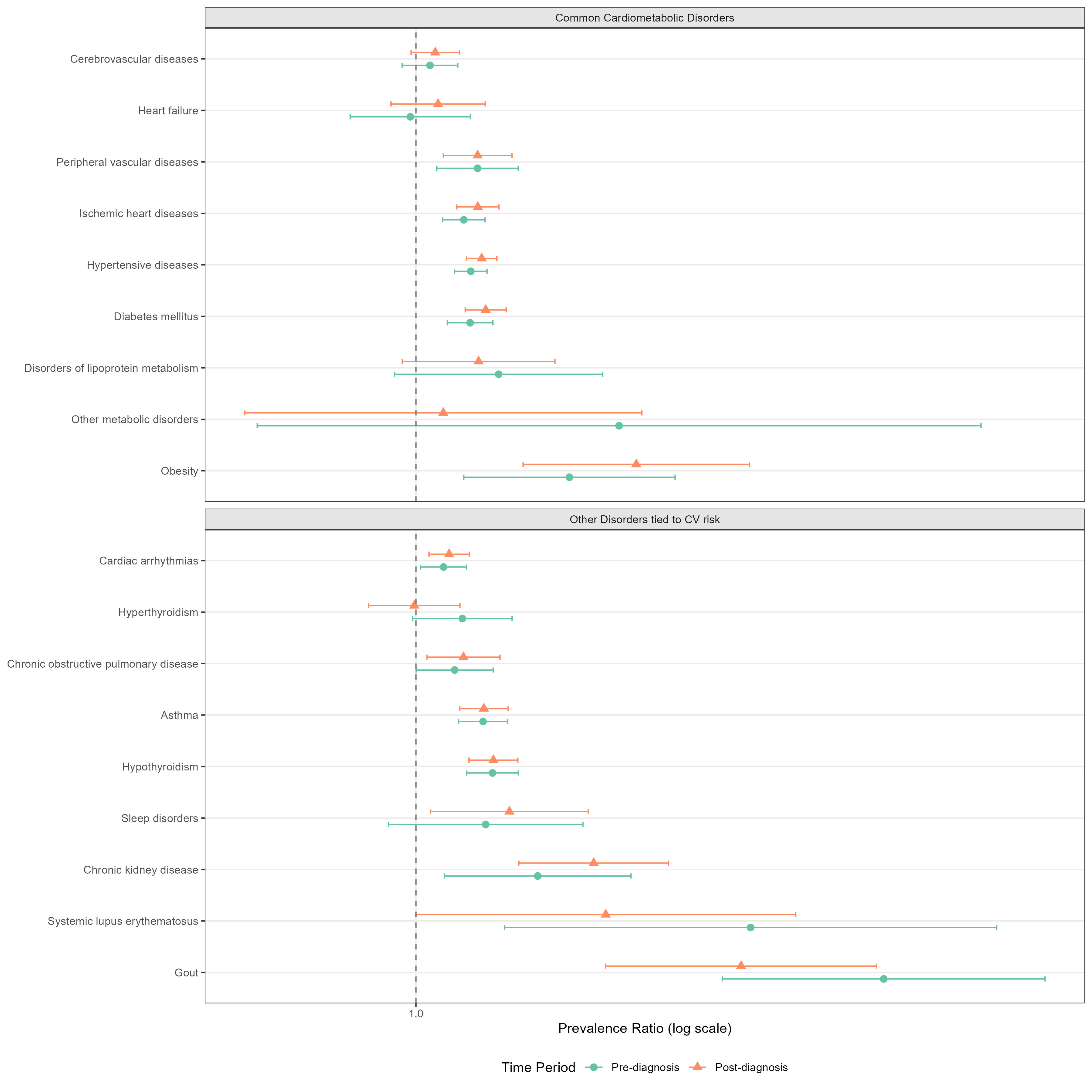
Temporal risk of various cardiometabolic disorders in patients with incident psoriatic arthritis as compared to the general population
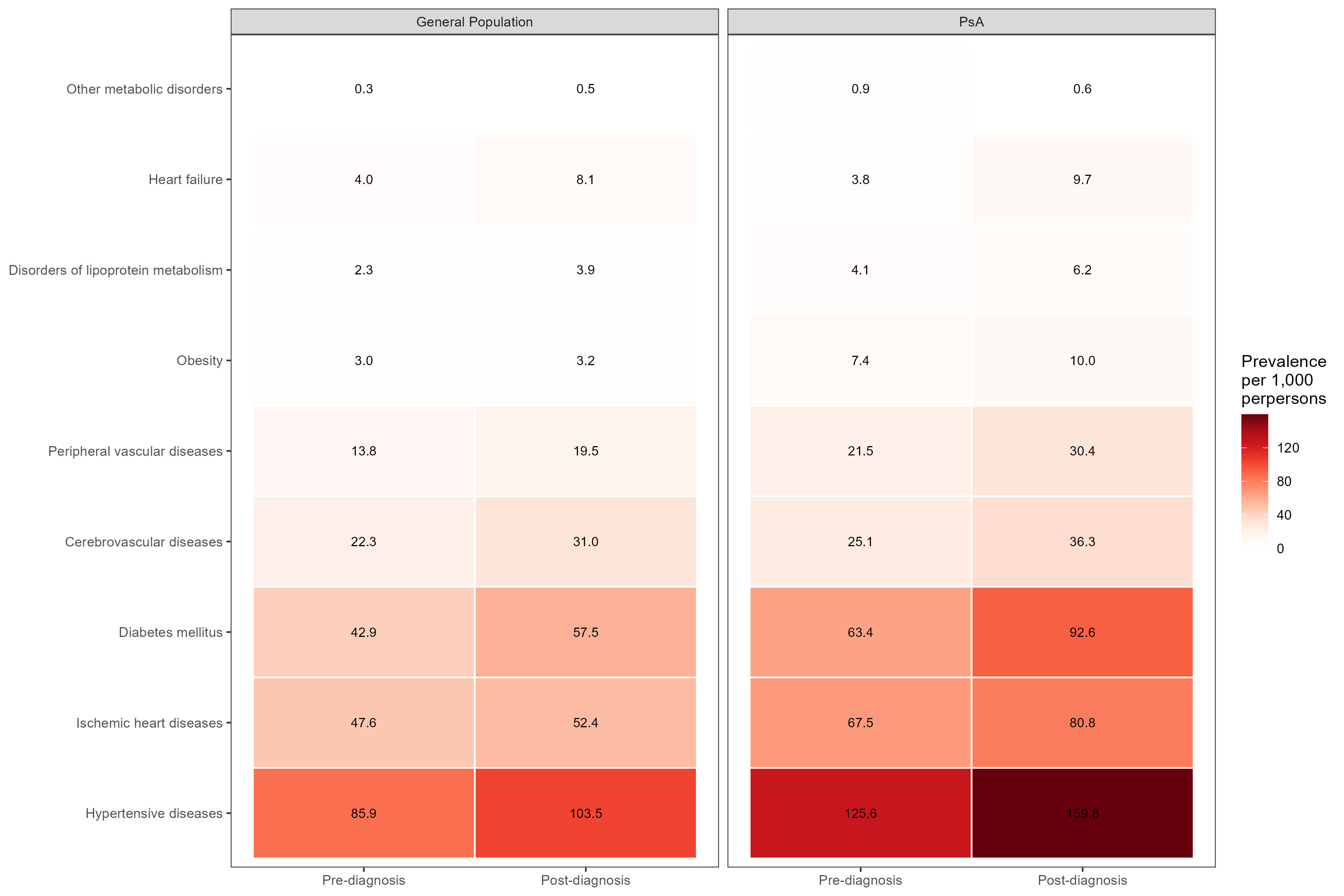
Heatmap for the overall burden of common cardiometabolic disorders in incident psoriatic arthritis patients and the general population
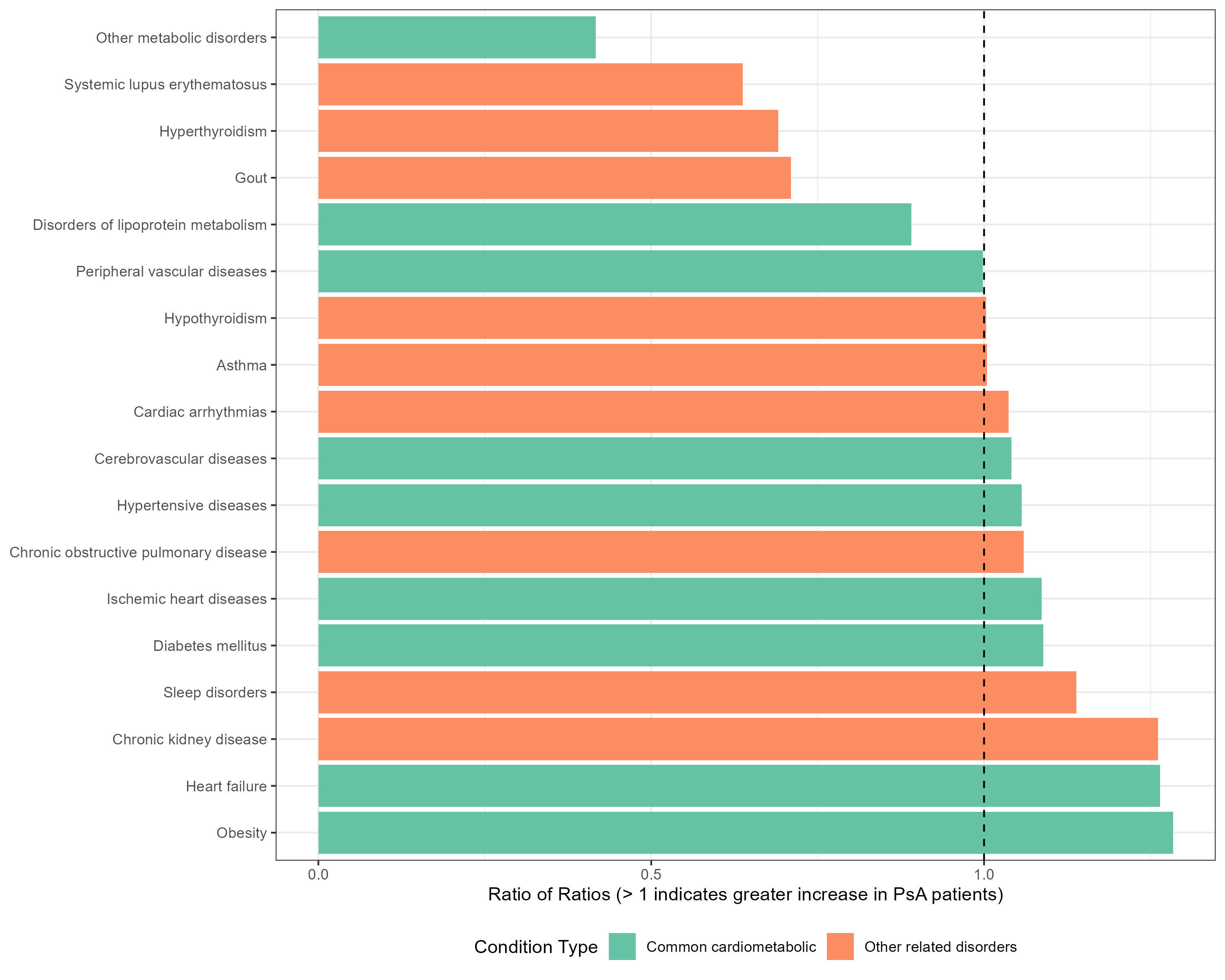
Temporal change in the burden of various cardiometabolic disorders in the five years after psoriatic arthritis diagnosis, as compared to the general population.
- BB
Abstract Poster Presenter(s)
Background/Purpose: While the association between psoriatic arthritis (PsA) and cardiometabolic disorders is established, the temporal sequence and progression of these comorbidities remain poorly characterized. To examine the temporal relationship between psoriatic arthritis (PsA) and cardiometabolic disorders by comparing their prevalence patterns before and after PsA diagnosis.
Methods: This nationwide retrospective case-control study analyzed Polish National Health Fund claims data (2011–2021). We identified 3,391 incident PsA patients diagnosed in 2016 using a definition requiring either: ICD-10 codes (M07.0-M07.3, L40.5) plus DMARD prescriptions, or ≥3 encounters with these codes in rheumatology settings. Cases were matched 1:10 to population controls by age, sex, and region. Cardiometabolic conditions (including hypertension, diabetes, ischemic heart disease, and metabolic disorders) were assessed based on ≥2 recorded diagnoses during five-year periods before and after PsA diagnosis.
Results: PsA patients demonstrated significantly elevated cardiometabolic risk both before and after diagnosis. Prevalence ratios (PR) were consistently higher across multiple conditions, with slight increases observed following diagnosis: hypertensive diseases (pre-PR 1.05 [95% CI 1.03–1.06] to post-PR 1.06 [1.04–1.07]), diabetes mellitus (pre-PR 1.05 [1.03–1.07] to post-PR 1.06 [1.04–1.08]), and ischemic heart diseases (pre-PR 1.04 [1.02–1.06] to post-PR 1.05 [1.03–1.07]). Notably, obesity showed the highest relative risk (pre-PR 1.13 [1.04–1.24] to post-PR 1.20 [1.09–1.32]). The mean cardiometabolic burden per patient increased by 34% following PsA diagnosis (from 0.32 to 0.43 conditions), with marked increases in heart failure (154%), lipoprotein disorders (50%), and diabetes (46%).
Conclusion: Temporal patterns in comorbidity of cardiovascular significance support the concept of shared inflammatory and metabolic pathways underlying these associations, highlighting the need for early cardiometabolic risk assessment and intervention in PsA management.

