Poster Session
Myositis
Poster Session B
Session: (1191–1220) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster II
1201: Prognostic Significance of 1-Year Pulmonary Function Changes in Myositis-Associated Interstitial Lung Disease
Monday, October 27, 2025
10:30 AM - 12:30 PM Central Time
Location: Hall F1
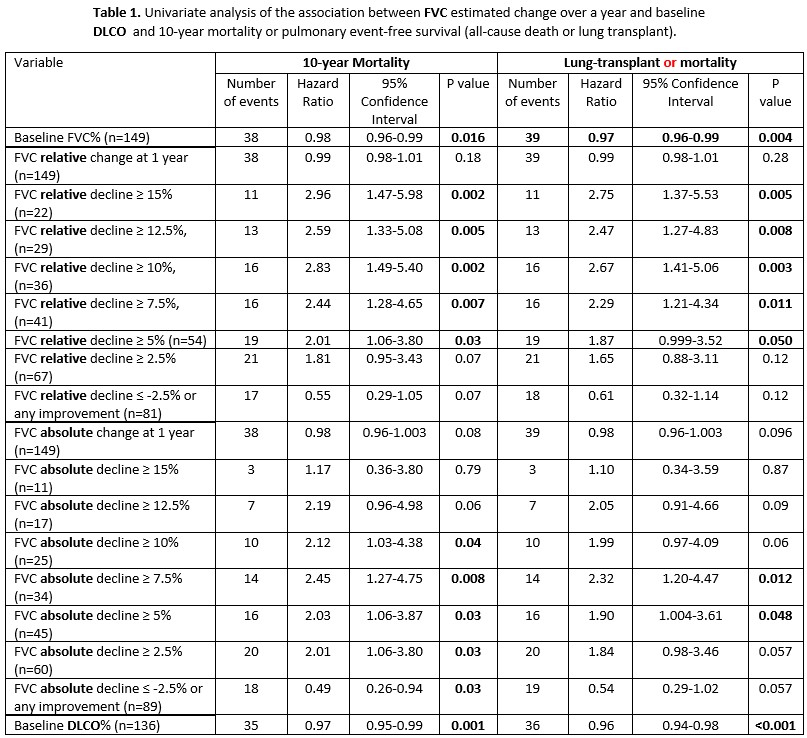
Table 1.
Association of One-Year FVC Change and Baseline DLCO with 10-Year Mortality and Transplant-Free Survival in IIM-ILD.
Univariate Cox regression analysis showing that absolute and relative FVC declines ≥5% were significantly associated with increased mortality and adverse outcomes. Baseline DLCO was also a strong predictor of transplant-free survival.
Association of One-Year FVC Change and Baseline DLCO with 10-Year Mortality and Transplant-Free Survival in IIM-ILD.
Univariate Cox regression analysis showing that absolute and relative FVC declines ≥5% were significantly associated with increased mortality and adverse outcomes. Baseline DLCO was also a strong predictor of transplant-free survival.
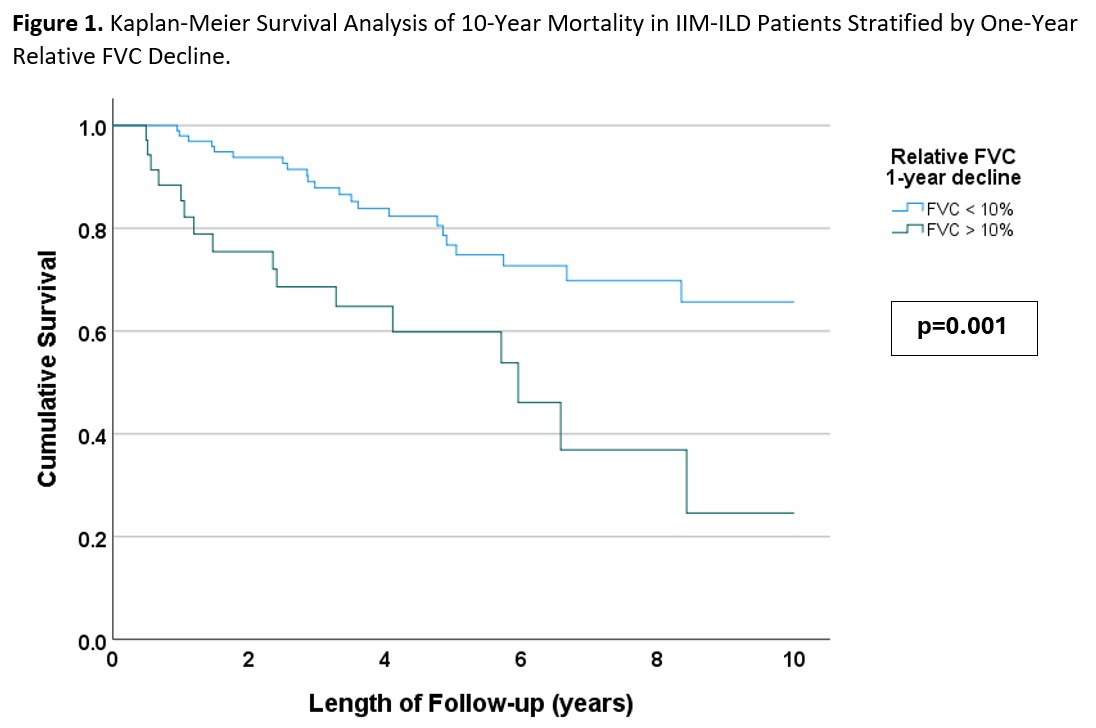
Figure 1.
Kaplan-Meier Survival Curves Stratified by One-Year Relative FVC Decline in IIM-ILD.
Patients with ≥10% relative FVC decline demonstrated significantly worse 10-year survival.
Kaplan-Meier Survival Curves Stratified by One-Year Relative FVC Decline in IIM-ILD.
Patients with ≥10% relative FVC decline demonstrated significantly worse 10-year survival.
- IC
Irada Choudhuri, MD
University of Pittsburgh Medical Center
Pittsburgh, Pennsylvania, United StatesDisclosure(s): No financial relationships with ineligible companies to disclose
Abstract Poster Presenter(s)
Background/Purpose: Lung involvement is the most frequent and severe extramuscular complication of Idiopathic Inflammatory Myopathy (IIM). The utility of pulmonary function test (PFT) monitoring for predicting long-term outcomes in IIM-associated interstitial lung disease (IIM-ILD) and assessing treatment efficacy in clinical trials remains unclear.
We aimed to evaluate the association between 1-year changes in PFTs and long-term outcomes, including 10-year mortality and lung transplant, in patients with IIM-ILD.
Methods: A prospective cohort of adult IIM-ILD patients was analyzed retrospectively. ILD was defined as per ATS criteria using chest HRCT, and myositis was classified according to either myositis-specific autoantibodies and/or the 2017 EULAR/ACR IIM classification criteria. Baseline was defined as the first rheumatology visit. Inclusion criteria required baseline and follow-up PFTs 6–18 months apart. Changes in forced vital capacity (FVC)% and diffusing capacity (DLCO)% were calculated as annualized values: [ΔFVC or ΔDLCO ÷ interval in months] × 12. Cox regression identified associations between PFT trends and outcomes, adjusting for age, sex, smoking, baseline FVC%, and interval from baseline to the first PFT. Kaplan-Meier analysis compared survival by FVC% trends, HRCT patterns, and IIM subsets.
Results: The study included 149 patients (mean age 50.5 ± 12.9 years, 63% female, 85% White). Based on serology, ASyS was the most frequent IIM subset (73.2%), followed by dermatomyositis (10.7%) and polymyositis (8.7%). Mean baseline FVC was 67.5 ± 19.3%, and DLCO was 54.2 ± 19.4%. The HRCT ILD pattern was nonspecific interstitial pneumonia (NSIP) in 85 (57.0%) patients, usual interstitial pneumonia (UIP) in 31 (20.8%) and organizing pneumonia in 2 (1.4%). After a median follow-up of 4.4 years, 41 (27.5%) had died and 6 (4%) had undergone lung transplant.
Both absolute and relative FVC declines of ≥5% over 1 year were significantly associated with higher mortality (HR 2.03 and 2.01; [p=0.03]) and lower transplant-free survival (HR 1.90 [p=0.048] and 1.87 [p=0.050]). Relative FVC declines ≥10% or ≥15% over 1 year showed even stronger associations with mortality (HR 2.83 [p=0.002] and 2.96 [p=0.002], respectively). Conversely, stable or improved absolute FVC was linked to lower mortality (HR=0.49, p=0.04). Baseline DLCO, but not its subsequent decline, was associated with transplant-free survival (HR 0.96, p< 0.001) (Table 1). Multivariate analysis revealed similar results. Survival was significantly worse among patients with relative FVC decline > 5%, > 7.5%, >10%, >12.5%, and > 15% (p < 0.05) (Figure 1). No significant differences in survival were observed between ASyS and other IIM subsets, or UIP and other HRCT patterns.
Conclusion: FVC decline, even at a threshold as low as 5%, is a significant predictor of long-term mortality and lung transplant in IIM-ILD. However, the 10% threshold, showing stronger associations with outcomes, should be incorporated as an outcome measure in IIM-ILD clinical trials. Routine PFT monitoring from IIM-ILD provides valuable prognostic information, enabling improved risk stratification and individualized treatment planning.

