Poster Session
Myositis
Poster Session B
Session: (1191–1220) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster II
1220: Predictors of Progressive Pulmonary Fibrosis in Idiopathic Inflammatory Myopathies : a Retrospective Study of 502 Cases
Monday, October 27, 2025
10:30 AM - 12:30 PM Central Time
Location: Hall F1
.jpg)
Table Comparisons in features at baseline between IIM-ILD patients with and without PPF
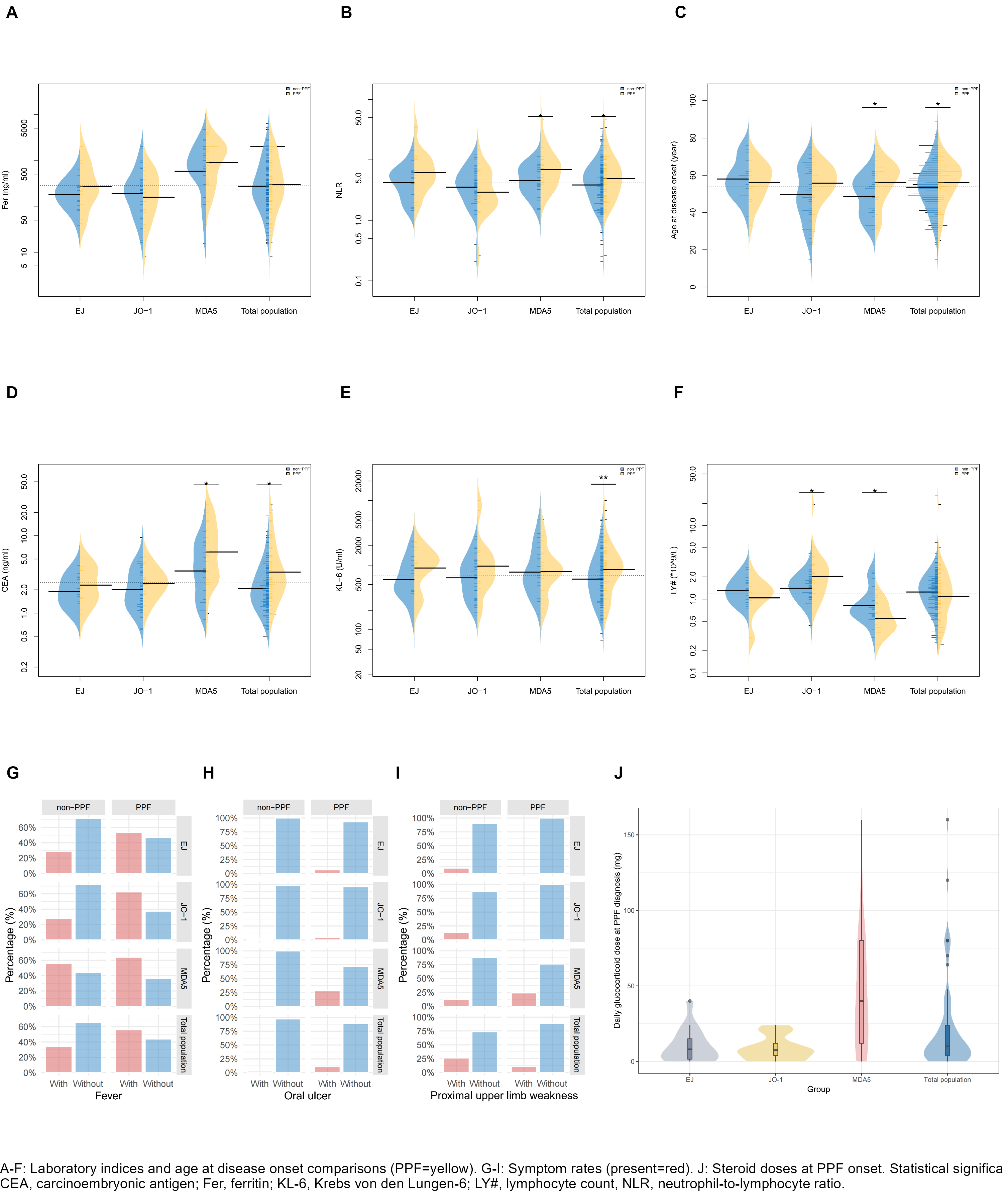
Figure PPF-associated features across IIM-ILD subtypes classified by MSA
- WB
Wei Bian, MD
Tianjin Medical University
Heping Qu, Tianjin, ChinaDisclosure(s): No financial relationships with ineligible companies to disclose
Abstract Poster Presenter(s)
Background/Purpose: Interstitial lung disease (ILD) in idiopathic inflammatory myopathies (IIM) causes worse prognosis. Some patients develop progressive pulmonary fibrosis (PPF) despite appropriate treatment. Identifying predictors of PPF in IIM patients is crucial for clinical management.
Methods: Patients with IIM hospitalization from 2015 to 2024 were retrospectively collected to identify factors associated with PPF using the American Thoracic Society, European Respiratory Society, Japanese Respiratory Society and Asociación Latinoamericana de Thórax guidelines PPF criteria published in 2022.
Results: ILD presented in 68.5% of IIM patients (344 /502). During follow up, 28.5% (82/288) developed PPF. The median interval from ILD diagnosis to PPF onset was 10 months. The median daily glucocorticoid dose methylprednisolone equivalents at PPF development was 10 mg, among anti-MDA5+ patients it was 40 mg (Figure). In IIM-ILD patients, the top three positive myositis-specific antibodies (MSAs) were anti-Jo-1 (24.1%), anti-MDA5 (21.5%) and anti-EJ (10.8%), and in IIM-PPF patients were anti-MDA5 (30.5%), anti-Jo-1 (29.3%) and anti-EJ (18.3%). Compared to non-ILD patients, those with ILD were older, more frequently anti-Ro52+ (73.3% vs. 39.2%, P< 0.001), and had higher Krebs von den Lungen-6 (KL-6), carcinoembryonic antigen (CEA) at baseline. Among IIM-ILD patients, PPF patients exhibited older age at onset, higher fever (56.1% vs. 34.5%, P=0.001) and oral ulcer prevalence (11% vs. 2.9%, P=0.014), higher CEA [2.83(1.92, 5.46) vs. 1.95(1.3, 3.27) ng/ml, P< 0.001], more frequent anti-MDA5+ (30.5% vs. 12.9%, P< 0.001), and ground-glass opacity on chest high-resolution CT (89% vs. 78%, P=0.032) (Table). In contrast, patients without PPF had higher anti-PL-7 positivity (11.4% vs. 2.4%, P=0.015), better diffusing capacity for carbon monoxide (58.78%±16.53% vs. 52.29%±15.66%, P=0.007), and more frequent MMF use (21.4% vs. 9.8%, P=0.021) (Table). KL-6 levels remained statistically comparable between baseline and time of PPF (P=0.23). CEA levels were higher in PPF group [2.83 (1.92-5.46) vs. 1.95 (1.30-3.27) ng/ml, P< 0.001] and longitudinal analysis revealed a marked increase from baseline to PPF [2.79(1.59-5.56) vs. 2.84(1.63-4.91) ng/ml, P=0.03]. Multivariate COX analysis identified fever [HR=2.21, 95%CI (1.39, 3.53), P=0.001], oral ulcer [HR=2.44, 95%CI (1.08, 5.50), P=0.031] and CEA [HR=1.11, 95%CI (1,05, 1.17), P< 0.001] as independently risk factors for PPF, while anti-PL7+ [HR=0.075, 95%CI (0.02, 0.36), P=0.001] and proximal upper limb weakness [HR=0.40, 95%CI (0.19, 0.85), P=0.017] as protective factors.
Conclusion: Manifestations of fever, oral ulcer and higher level of CEA at baseline were independently risk factors for PPF, especially among patients with specific autoantibodies. Close monitor of patients' symptom progression and timely scheduling of chest HRCT and PFTs are necessary, when daily glucocorticoid dose tapering to about 10 mg methylprednisolone equivalent. CEA level at baseline may represent a more promising biomarker candidate for identification of PPF.

