Poster Session
Epidemiology, Health Policy, and Outcomes
Poster Session B
1645: A Sex-modified Association Between Perfluoroalkyl and Polyfluoroalkyl Substances (PFAS) Blood Concentration and Prevalent Arthritis Among Young and Middle-aged US Adults
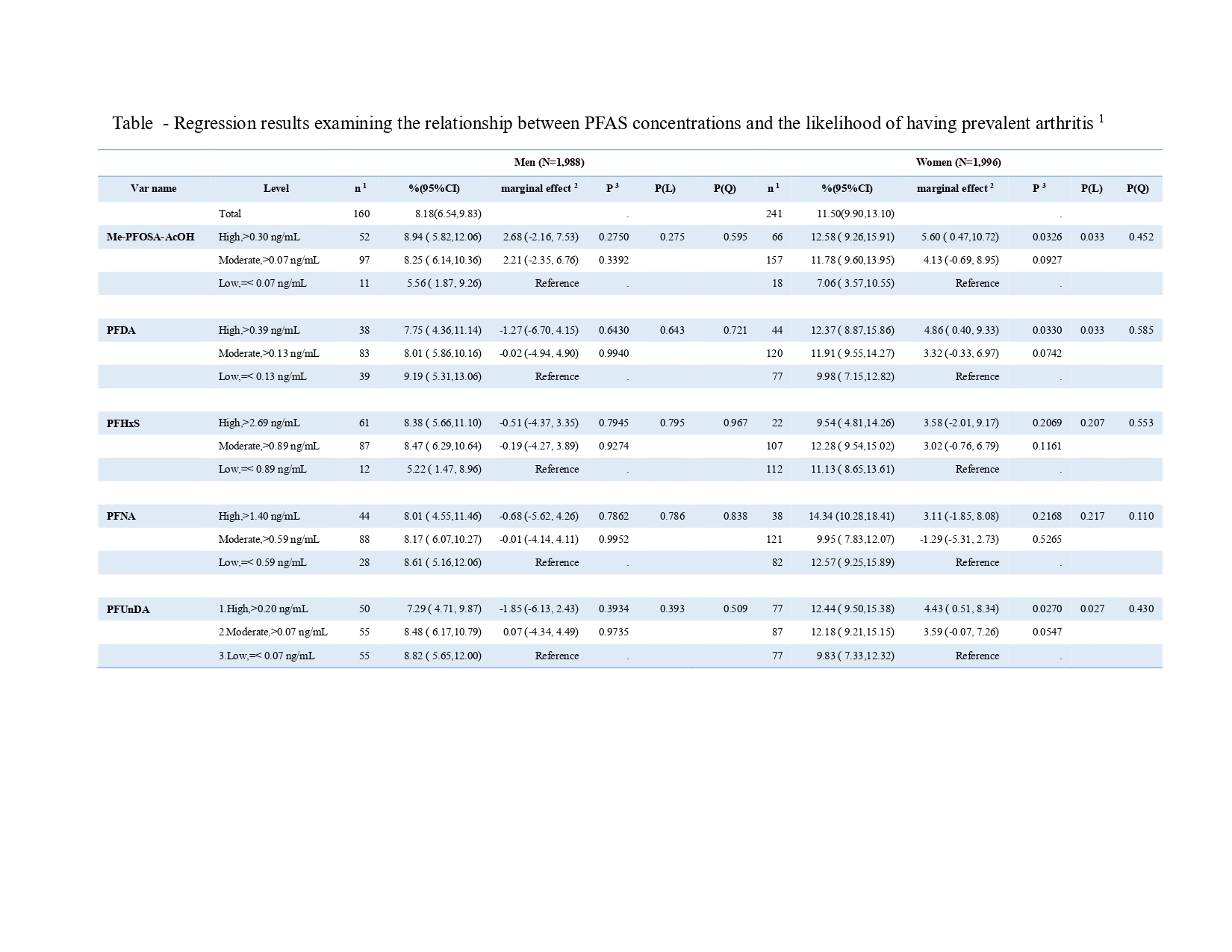
1. The case numbers of arthritis.
2. Estimated with fixed effect. The marginal effect indicates the predicted change in the percentage of adults with a high-level body weight or height associated with a high level of PFAS compared to a low level, holding the covariates at their mean value.
3. The p-value for the marginal effect against the reference level (difference > 0).
- QE
Queeneth Edwards, MD, MPH
Georgia Southern University
Statesboro, Georgia, United StatesDisclosure(s): No financial relationships with ineligible companies to disclose
Abstract Poster Presenter(s)
Background/Purpose:
Perfluoroalkyl and Polyfluoroalkyl Substances (PFAS) (PFAS), including Perfluorooctanoic acid (PFOA) and Perfluorooctane sulfonate (PFOS), are persistent environmental contaminants that may influence inflammatory joint diseases by altering immune function and promoting chronic inflammation. While studies on PFAS and rheumatoid arthritis risk have yielded mixed results, likely due to methodological flaws like misapplied odds ratios. We estimated the marginal effect of PFAS exposure on arthritis diagnosis among young and middle-aged U.S. adults.
Methods:
We analyzed data from 3,984 participants aged 20-49 years in the 2005–2020 nationally representative survey, using surplus sera collected for cotinine testing. Analyses were limited to the five PFAS measured continuously during this period among eligible participants: 2-(N-methyl-PFOSA) acetic acid (Me-PFOSA-AcOH), Perfluorodecanoic acid (PFDA), Perfluorohexane sulfonic acid (PFHxS), Perfluorononanoic acid (PFNA), and Perfluoroundecanoic acid (PFUA).Marginal effects on prevalence of doctor-diagnosed arthritis were estimated by comparing high (4th quarter) and moderate (2nd–3rd quarter) PFAS exposure to low (1st quarter) level exposure. Potential confounders adjusted for included age (modeled as a continuous variable), race/ethnicity, family income, history of major chronic diseases (including cardiovascular diseases, diabetes, and cancer), and body mass index.
Results: The overall prevalence of arthritis was 9.80% (standard error = 0.57%), with 401 cases identified. Among men, neither a significant association nor a clear pattern was observed across the five PFAS analysed. Specifically, the prevalence of arthritis was 8.94% (95% CI: 5.82%, 12.06%), 8.25% (6.14%, 10.36%), and 5.56% (1.87%, 9.26%) for those with high, moderate, and low concentrations of Me-PFOSA-AcOH, respectively. The adjusted marginal effect (ME) for high Me-PFOSA-AcOH was 2.68 (95% CI: -2.16, 7.53) relative to low PFAS concentration, while for high PFUnDA it was -1.85 (95% CI: -6.13, 2.43).
In contrast, a clear pattern of association emerged among women, with statistically significant findings for some PFAS. Among women, the prevalence of arthritis was 12.58% (95% CI: 9.26%, 15.91%), 11.78% (95% CI: 9.60%, 13.95%), and 7.06% (95% CI: 3.57%, 10.55%) for high, moderate, and low concentrations of Me-PFOSA-AcOH, respectively. The adjusted MEs were 5.60% (95% CI: 0.47%, 10.72%) for those with high levels and 4.13% (95% CI: -0.69%, 8.95%) for those with moderate levels compared to women with low levels, with a significant linear trend (p = 0.033). Similar statistically significant associations were observed for PFDA and PFUnDA, whereas the associations for PFHxS and PFNA did not reach statistical significance.
Conclusion: High levels of PFAS were associated with an increased prevalence of arthritis among women, but not among men. The distinct susceptibility suggests that differences in hormonal or metabolic responses to these persistent chemicals may underlie the association. These findings warrant further longitudinal and mechanistic studies

