Poster Session
Epidemiology, Health Policy, and Outcomes
Poster Session B
1635: Association Between Treatment Adherence and Frailty in Patients with Rheumatic Diseases
- DG
Daniela L. Guillen-Tejada, MD
Universidad de las Américas Puebla
Puebla, Puebla, MexicoDisclosure(s): No financial relationships with ineligible companies to disclose
Abstract Poster Presenter(s)
Background/Purpose: Management of rheumatic diseases relies on chronic treatment, often with a greater risk of nonadherence. Frailty is characterized by decreased physiological function that increases patients’ vulnerability. Frailty is more prevalent in patients with rheumatic diseases than in healthy controls. Nonadherence to treatment and its complications can lead to frailty. The purpose of this study is to determine an association between treatment adherence and frailty in patients with rheumatic diseases. It is crucial to identify contributing factors to the development of frailty to propose interventions aimed at decreasing the risk of related adverse outcomes.
Methods:
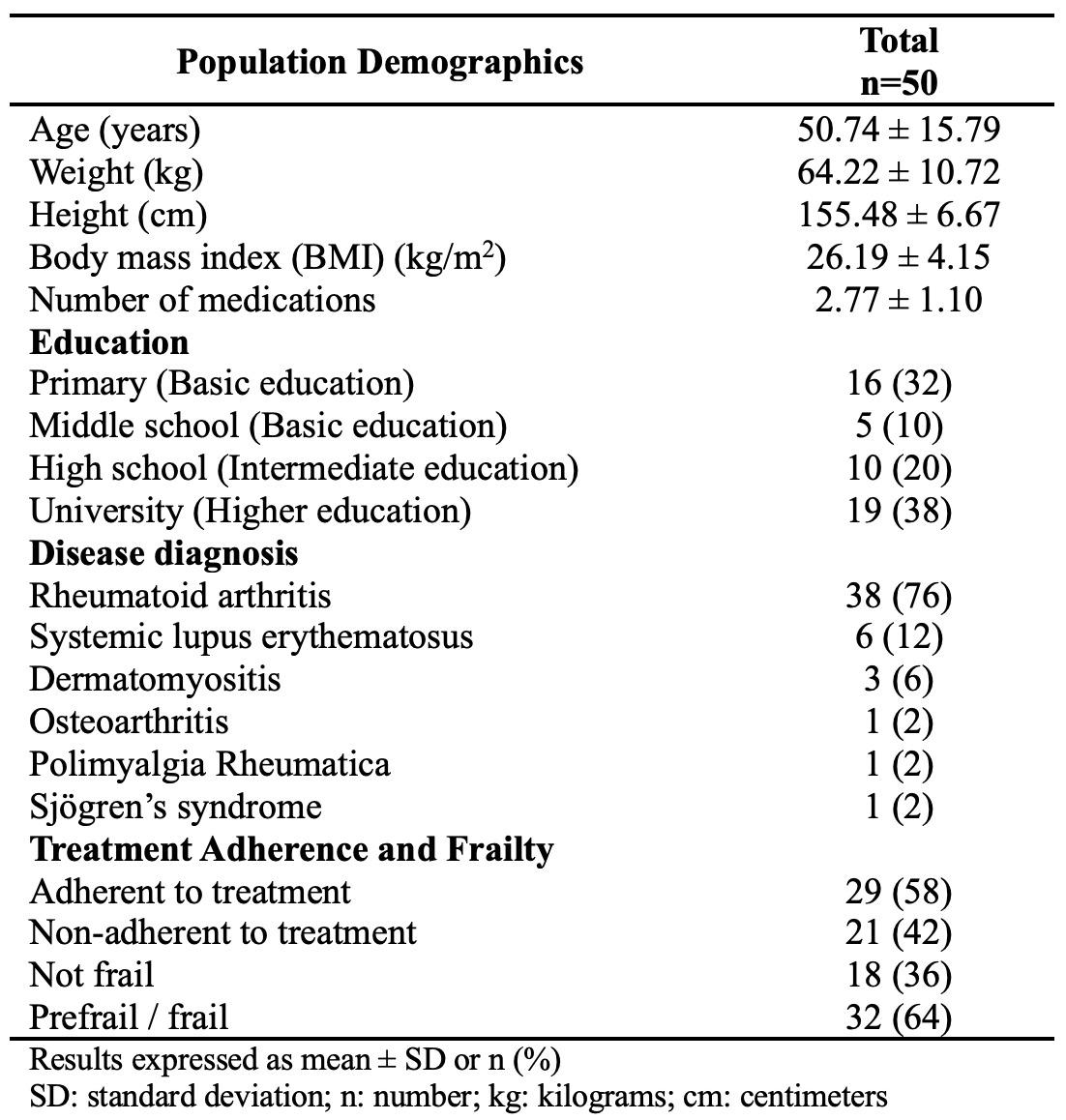
This study is a cross-sectional study in a population of 50 adult female patients with rheumatic diseases under treatment, for 2 or more months prior to their participation. All patients satisfied ACR classification criteria for diagnosis. Patients were interviewed once during follow-up appointments. The Voils DOSE-Nonadherence measure assessed treatment adherence. Fried’s Frailty Phenotype was used to assess frailty status.
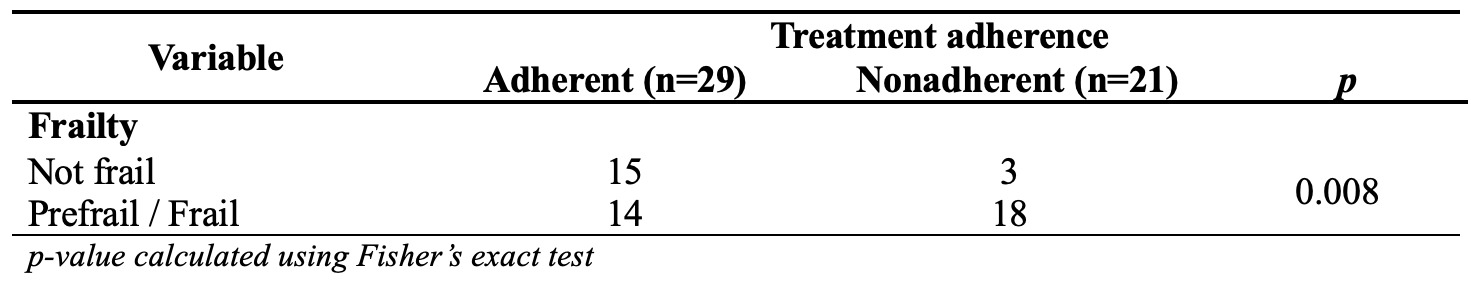
Descriptive statistics were used to evaluate treatment adherence; compare the degree of adherence in various rheumatic diseases; establish the reasons for treatment nonadherence; determine frailty status; compare frailty status with age and etiology; and determine the relationship between adherence and frailty. To analyze association, Fisher’s exact test, Student T-test, and chi-square were used.
Results:
The population consisted of 50 patients with a mean age of 50.74 years. 42% had a basic level of education and 58% had an intermediate or higher education. Out of all patients, 76% are diagnosed with RA; 12% with SLE; 6% with DM; 2% with PMR; and 2% with SS. 58% of the patients were adherent to treatment for their disease. 64% of patients were prefrail or frail.
Among RA patients, 58% were adherent to treatment. 66% of RA patients were prefrail or frail. Of the 6 SLE patients, 67% were adherent to treatment. 50% of SLE patients were prefrail or frail. The main reasons for nonadherence were forgetfulness; not having the medication with them; not being able to get answers to questions about the medication; and because they ran out of medication.
Regarding treatment adherence and its association with frailty, out of 29 patients who were adherent to treatment, 15 were not frail. Of the 21 nonadherent patients, 18 were prefrail or frail. There is an association between treatment adherence and frailty in patients with rheumatic diseases (p = 0.008).
Conclusion: Frailty decreases physiological reserve in response to stress, resulting in higher vulnerability to adverse outcomes. Treatment adherence is the degree to which patients follow prescribed treatment. An association has been established between treatment adherence and increased risk of frailty in a group of 50 patients with rheumatic diseases. Special focus should be given to develop interventions that improve treatment adherence to reduce the risk of developing frailty and prevent associated consequences.

