Poster Session
Epidemiology, Health Policy, and Outcomes
Poster Session B
1648: Predicting Worse Disease Activity, QOL, and Progression to Advanced Therapies at 12 and 24 months in Early RA: Results from the Canadian Early Arthritis Cohort (CATCH)
- SB
Susan Bartlett, PhD
McGill University
Montreal, QC, CanadaDisclosure(s): Accord Health: Consultant (Ongoing); Nordic: Consultant (Ongoing); Sanofi: Consultant (Terminated, May 1, 2025)
Abstract Poster Presenter(s)
Background/Purpose: Pain, fatigue, and emotional distress are common in new RA patients. It is unclear whether co-occurring symptoms predict worse outcomes and progression to advanced therapies in ERA. We compared the likelihood of biologics and JAKi use by 12 and 24 months by pain, fatigue, anxiety, and depression at diagnosis and after 3 months of MTX.
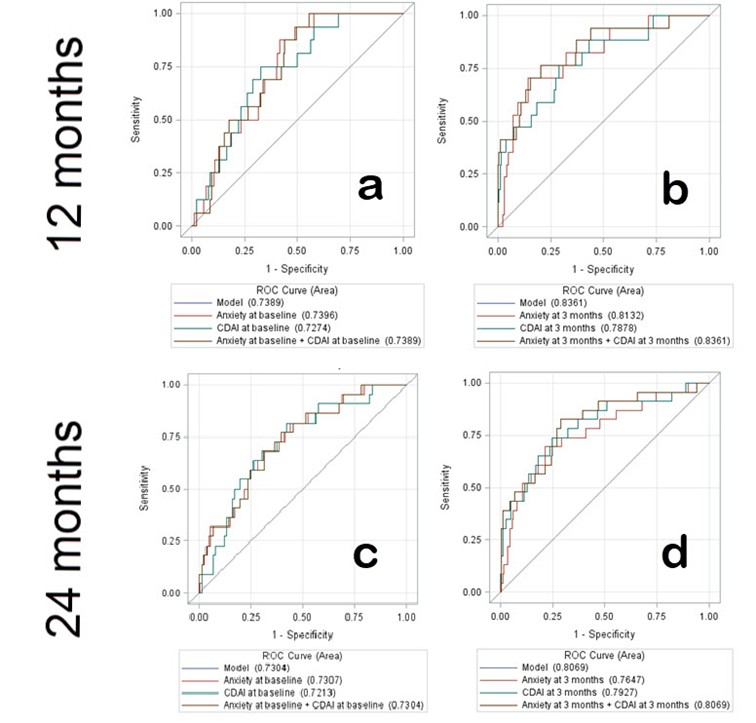
Methods: Data were from new RA patients enrolled in the Canadian Early Arthritis Cohort (CATCH) between 1/17-8/22 with active disease and on MTX. Participants underwent clinical assessments and completed PROMIS-29 at 0 and 3 months. Anxiety, depression, fatigue, and pain interference were defined as PROMIS ≥ 55. Multivariable logistic regression models and ROC curves for baseline and 3 months were constructed adjusting for CDAI, age, sex, race, education, smoking, obesity, comorbidities, serology and symptom duration.
Results:
The 255 adults had a mean (SD) age of 56 (14), and were mostly women (69%), White (78%) with a CDAI of 30 (14) at diagnosis. All started MTX monotherapy [55%] or with csDMARDs [45%].
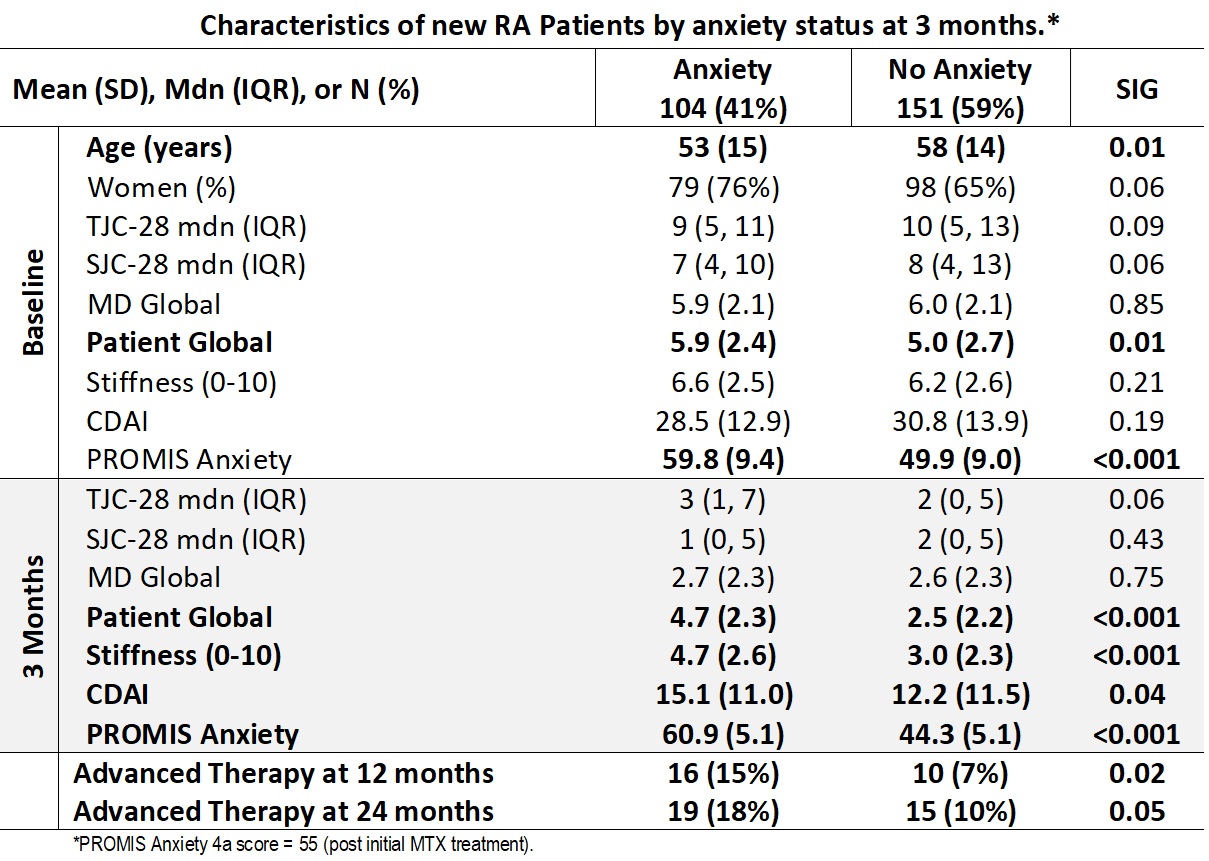
At 3 months, mean CDAI had improved substantially in all; more patients reported anxiety than at baseline (59% vs. 40%). As compared with baseline, 28 (11%) reported new anxiety while 49 (19%) were no longer anxious at 3 months. Mean Pain Interference, Fatigue, Anxiety and Depression scores also were 8-15 points higher in anxious vs. non-anxious patients.
By 12 months, more than twice as many patients who were anxious at 3 months (vs. non-anxious) were on advanced therapies (15% vs. 7%); a similar trend was observed at 24 months (18% vs. 10%). In contrast, the proportion of patients on advanced therapies were similar by pain interference, fatigue, or depression status at 3 months.
The optimal multivariable model for predicting advanced therapy use by 12 months included Anxiety status and CDAI at 3 months after adjustment for baseline age, sex, race, education, smoking status, obesity, comorbidities, serology status and symptom duration (Figure b; ROC 0.84 vs. 0.73 at baseline). Patients who were anxious at 3 months had 5.1 the odds (95% CI 1.4, 18.2) of being on advanced therapy at 1 year, with a similar trend at 24 months (OR 3.0; 95% CI 1.1, 8.2). In contrast, Depression, Pain interference, and Fatigue status at 3 months were not associated with a greater likelihood of progression to an advanced therapy by 12 and 24 months (data not shown). At baseline, the 138 (49%) who reported anxiety at 3 months were significantly (p< .01) younger and had higher patient global scores (Table).
Conclusion:
In this large real world longitudinal cohort of new RA patients, almost half reported anxiety at baseline, increasing to 59% by 3 months, even after a robust response to MTX treatment. A novel finding is that patients with anxiety at 3 months (but not higher levels of depression, fatigue, or pain interference) had worse CDAI disease activity and PROs, and a much greater odds of progressing to advanced therapies by 12 and 24 months. Anxious patients may be more likely to advocate for a change of treatment including advanced therapies; anxiety may also reflect a greater impact of social determinants of health. Better understanding of anxiety in early RA may offer new opportunities to improve QOL and support treatment decision making.

