Poster Session
Reproductive Health
Poster Session C
Session: (2195–2226) Reproductive Issues in Rheumatic Disorders Posters
2198: Sociocultural Influences on Pregnancy Planning for Individuals Diagnosed with SLE in an Urban Hispanic Population: A Qualitative Study with Considerations for a Holistic Approach
Tuesday, October 28, 2025
10:30 AM - 12:30 PM Central Time
Location: Hall F1
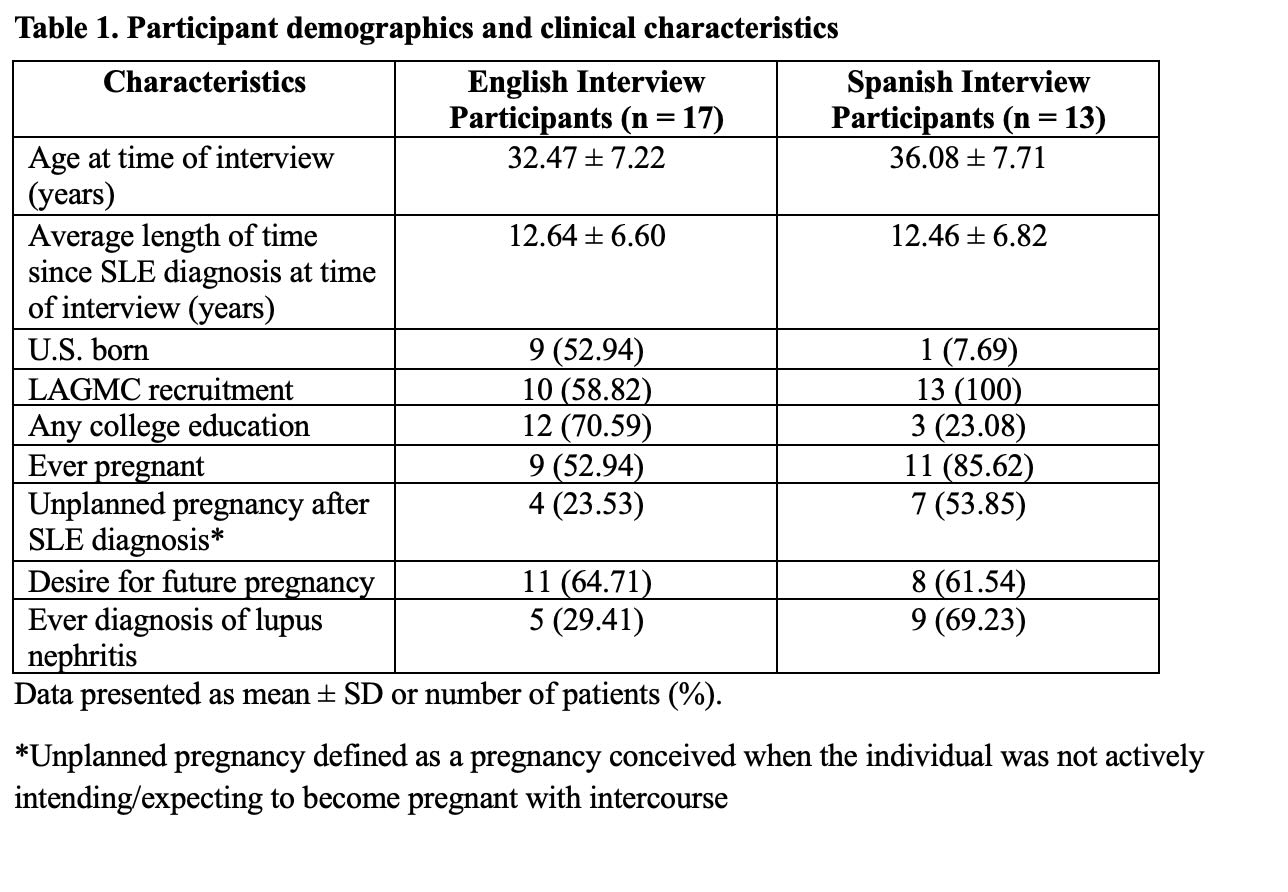
Table 1. Participant demographics and clinical characteristics
.jpg)
Table 2. Themes, subthemes, and representative quotes from grounded theory analysis on sociocultural influences for pregnancy planning
- LW
Leanna Wise, MD, MPH
LAGMC/Keck Medicine of USC
Pasadena, California, United StatesDisclosure information not submitted.
Abstract Poster Presenter(s)
Background/Purpose: As systemic lupus erythematosus (SLE) often affects women of child-bearing age, understanding how this population makes reproductive health decisions is critical for well-rounded healthcare. Individuals often need more than just SLE medical optimization to feel comfortable with attempting pregnancy; many extrinsic, non-medical factors play a role. In this qualitative thematic analysis study, we explored the perspectives of female participants of Hispanic ethnicity diagnosed with SLE to understand sociocultural non-clinical factors that influence pregnancy planning and contraception use.
Methods: We conducted a qualitative study using semi-structured interviews with 30 Hispanic women diagnosed with SLE, recruited from Los Angeles General Medical Center and LupusLA. Eligible participants were aged 18–45, of Hispanic ethnicity, sexually active with a male partner or considering pregnancy within three years, and fluent in English or Spanish. Interviews were conducted virtually in the participant’s preferred language, recorded, and transcribed; Spanish interviews were translated into English. Interviews were conducted from June 2024 – March 2025. Sociocultural influences were collected via interview questions asking what non-clinical factors play a role in participants’ decision-making to attempt pregnancy and/or use contraception, with a focus on participants' significant others, family, and sociocultural background. Data collection continued until thematic saturation was reached, and transcripts were analyzed using a grounded theory approach to identify sociocultural themes related to reproductive health decision-making. Coding was conducted by a multilingual, multidisciplinary team.
Results: A total of 17 English-speaking participants and 13 Spanish-speaking participants were interviewed (Table 1). Four sociocultural themes (Table 2) arose in both language groups which strongly influence patients’ views on pregnancy: 1) financial/career security; 2) support of their family (significant others and extended family support); 3) underlying cultural or religious beliefs (largely being against termination for unexpected pregnancy unless absolutely necessary, as well as divine control of the reproductive journey; 4) virtual media (a spectrum of both positive/negative influence). These themes emerged consistently among both English- and Spanish-speaking participants.
Conclusion: For women diagnosed with SLE, addressing reproductive health decision-making requires the clinician to approach the patient from a holistic perspective that considers the complex social and cultural factors influencing pregnancy decisions. While many patients with SLE should be timing pregnancy to be medically safe, our patient-reported qualitative data also demonstrates that pregnancy planning (or avoiding) is heavily influenced by non-medical extrinsic factors. Clinicians who acknowledge and address these factors may be better equipped to support patients in navigating pregnancy planning safely and confidently, promoting shared decision-making that aligns with patients’ lived experiences and values.

