Poster Session
Epidemiology, Health Policy, and Outcomes
Poster Session C
Session: (1972–1989) Measures & Measurement of Healthcare Quality Poster II
1987: Evaluating User Engagement and Real-World Impact of a PMR-Specific Digital Symptom Assessment Tool: A 12-Month Analysis of PainSpot™
Tuesday, October 28, 2025
10:30 AM - 12:30 PM Central Time
Location: Hall F1
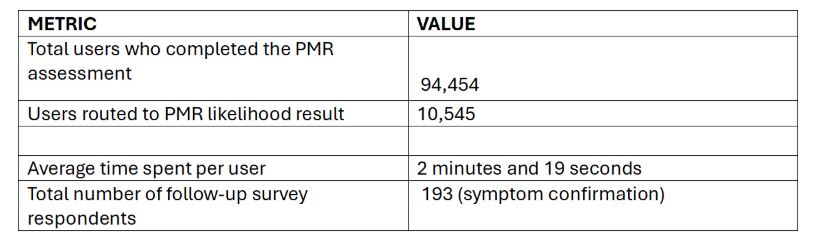
Table 1: PainSpot (TM) PMR Pathway User Engagement Overview
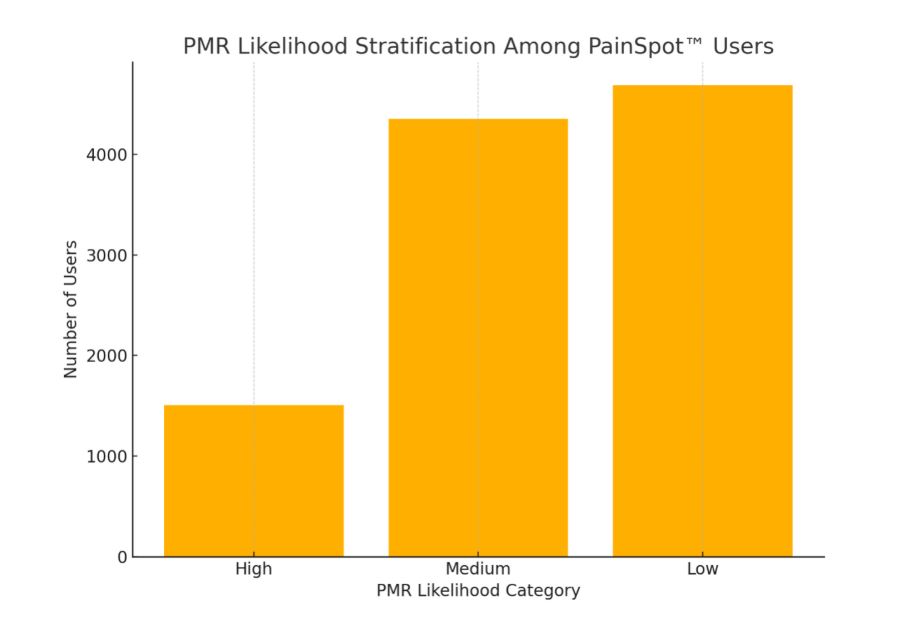
Figure 1: PMR Likelihood Stratification Among PainSpot Users
- SV
Shilpa Venkatachalam, PhD;MPH
Global Healthy Living Foundation
New York, New York, United StatesDisclosure information not submitted.
Abstract Poster Presenter(s)
Background/Purpose: Polymyalgia rheumatica (PMR) is a systemic inflammatory condition affecting individuals over 50, marked by bilateral shoulder and hip stiffness and pain. Its nonspecific symptoms and overlap with other musculoskeletal disorders often lead to diagnostic delays and misclassification, contributing to avoidable morbidity. Awareness of PMR remains limited, especially outside of rheumatology. Digital tools, such as algorithm-based symptom checkers, offer a scalable approach to identifying PMR-consistent symptom patterns and prompting medical evaluation. To address this gap, the PainSpot™ platform was enhanced with a PMR-specific pathway co-developed by clinicians and patients. This study assessed real-world tool engagement, diagnostic likelihood distribution, and user-reported outcomes.
Methods: PainSpot™ was modified to include a PMR-specific algorithm co-developed by a multi-stakeholder working group including rheumatologists, outcomes researchers, and patients with confirmed PMR diagnoses. Thirteen condition-specific questions were generated and refined through a literature review, clinical input, and patient interviews focusing on pre-diagnosis symptom recall. Between March 1, 2024, and February 28, 2025, user-level engagement data were collected and analyzed to evaluate assessment completion rates, PMR likelihood results, and follow-up survey responses.
Results: Of 94,454 users who completed the PainSpot™ assessment between March 2024 and February 2025, a subset were routed to a potential PMR result based on algorithmic analysis of symptom patterns. Among these, 1,509 users (21.0%) were classified as high likelihood of PMR, 4,353 (60.6%) as medium likelihood, and 4,683 (65.2%) as low likelihood. These stratifications were derived from a weighted question algorithm developed through clinician and patient input. Average engagement time across users was 2 minutes and 19 seconds, indicating sustained interaction with the digital interface. Follow-up surveys were administered to users who completed the assessment. Among 111 respondents, 89.2% (n=99) reported discussing their results with a healthcare provider, suggesting potential influence on care-seeking behavior. Additionally, 193 assessment completers (across all diagnostic pathways, not limited to PMR) responded to a separate follow-up question regarding the accuracy of the tool’s output; 82.4% (n=159) indicated that the result they received aligned with their symptom experience or was subsequently confirmed.
Conclusion: The PMR-specific pathway within PainSpot™ demonstrated high engagement meaningful stratification of diagnostic likelihood, and strong perceived utility based on user-reported outcomes.. While only a subset of users confirmed seeking medical follow-up, a larger proportion—over 80% of survey respondents—indicated that the tool’s output aligned with their symptom experience. These findings support the utility of patient-informed, algorithm-based tools in recognizing symptom patterns consistent with PMR. This work aligns with a four-year CDC-funded initiative aimed at improving national awareness, education, and diagnostic strategies for PMR.

