Poster Session
Epidemiology, Health Policy, and Outcomes
Poster Session B
Session: (1038–1054) Health Services Research Poster II
1047: Primary Care Perspectives on Giant Cell Arteritis: Diagnostic Considerations, Referral Challenges, and Opportunities for Fast-Track Pathways in the U.S.
Monday, October 27, 2025
10:30 AM - 12:30 PM Central Time
Location: Hall F1
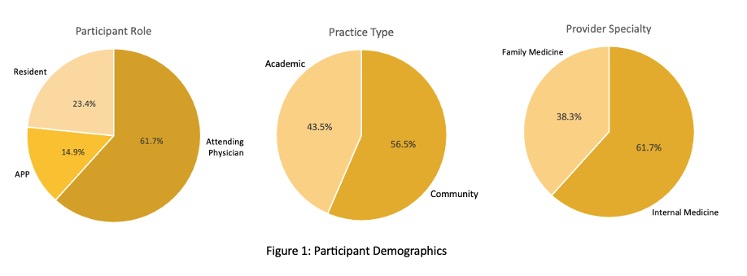
Figure 1 - Participant Demographics
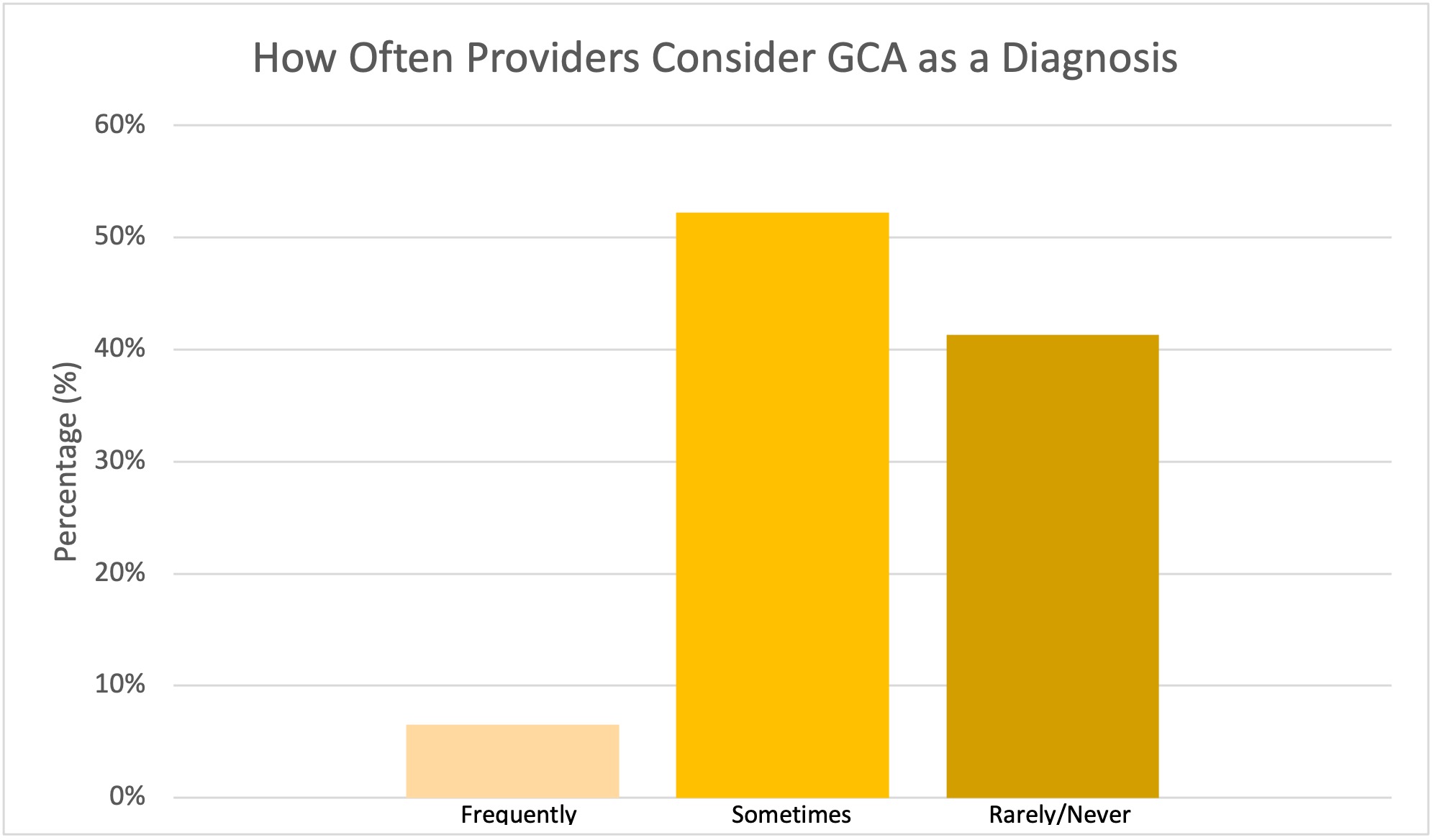
Figure 2 - Frequency Providers Consider GCA as a Diagnosis
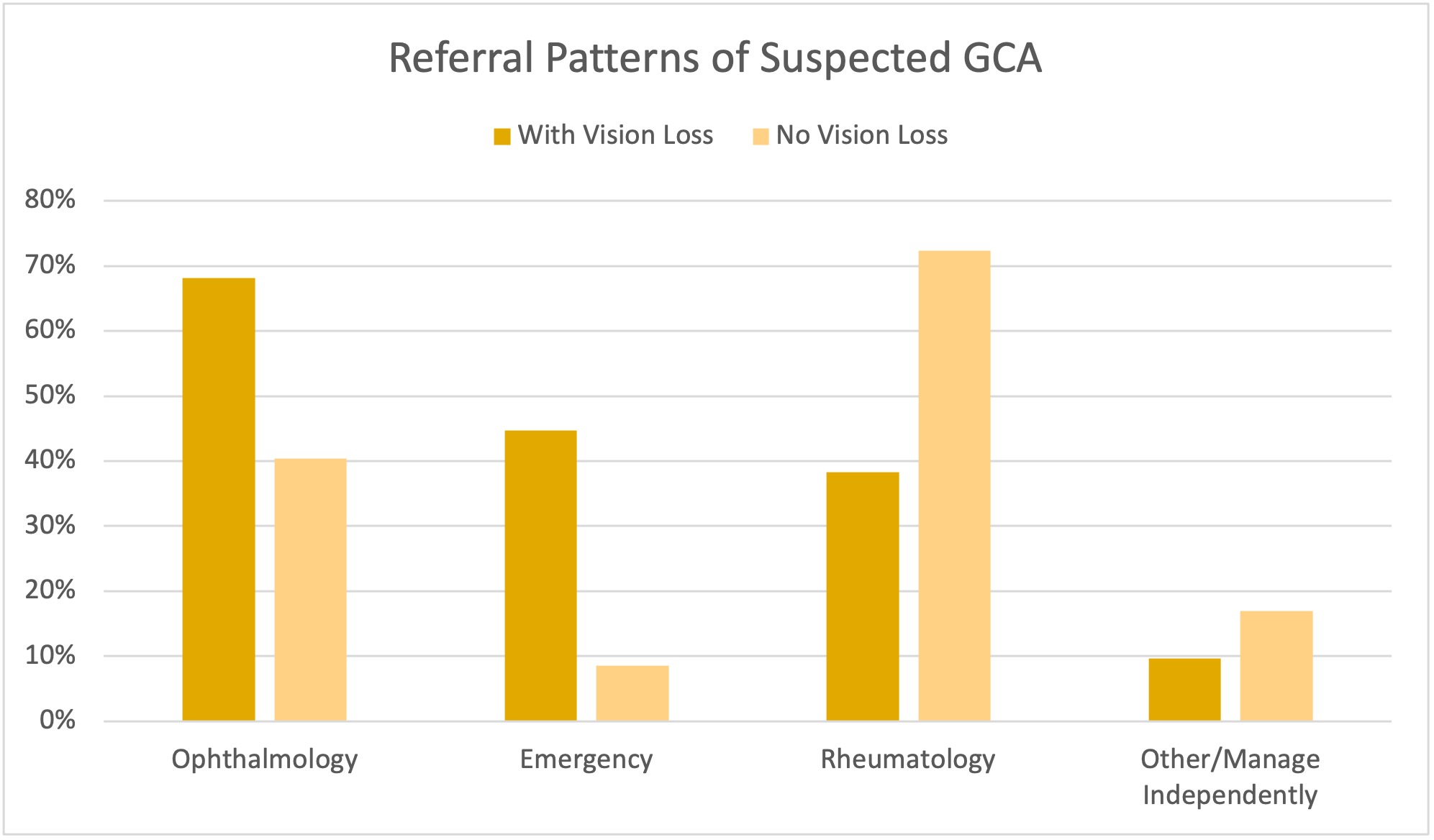
Figure 3 - Referral Patterns for Suspected GCA
- JG
Jon Golenbiewski, DO
Wake Forest University School of Medicine
Winston-Salem, North Carolina, United StatesDisclosure information not submitted.
Abstract Poster Presenter(s)
Background/Purpose: Giant Cell Arteritis (GCA) is a medical emergency that can lead to irreversible vision loss without prompt recognition and treatment. Primary care providers (PCPs) often serve as the initial evaluators of suspected GCA. To date, no U.S. study has evaluated how PCPs approach GCA evaluation and management. This study aims to understand PCPs’ perspectives, diagnostic and referral practices, and barriers they face in managing suspected GCA—highlighting opportunities to streamline subspecialty care and reduce risk for adverse outcomes.
Methods: A 35-question electronic survey was distributed to 350 PCPs as part of a large health system in central North Carolina. The survey explored awareness of GCA, diagnostic tools, treatment approaches, referral workflows, and perceptions of system-level challenges. Responses were analyzed descriptively.
Results: Forty-seven providers responded (13.4% response rate), including internal medicine and family medicine providers in academic (56.5%) and community (43.5%) settings. Most respondents (n=42, 89.2%) would sometimes or rarely consider GCA as a possible diagnosis. Confidence in diagnosing GCA was moderate with a mean of 6.2 (95% CI = 5.7 - 6.7) and slightly lower for management with a mean of 5.2 (95% CI = 4.6 - 5.8). Eighty percent of providers (n=38) initiate high dose glucocorticoids (≥1 mg/kg) when GCA is suspected with 58.3% (n=27) of respondents continuing until specialist evaluation. Most respondents referred to specialists for management of GCA; however, 2.1% (n=1) of PCPs manage patients independently. Over half (n=29, 63%) were unaware of biologic therapies as treatment options for GCA.
Referral pathways varied: 68.1% (n=32) referred to ophthalmology when vision loss was suspected, yet only 44.7% (n=21) involved the emergency department. Wait times to see rheumatology were frequently prolonged, with 51.1% (n=24) reporting delays greater than 4 weeks. Coordinating referrals was cited as difficult by 75.6% (n=35) of respondents, often requiring extra time and resources to have patients evaluated. Communication is rare among referring providers as only 19.1% (n=9) reported direct communication with an on-call provider. Respondents expressed strong interest (n=45, 95.7%) in a fast-track clinic or protocol to improve triage and access for suspected GCA cases.
Conclusion: This is the first U.S.-based study to explore primary care experiences in managing suspected GCA. Our study highlights that GCA remains an infrequently considered diagnosis amongst PCPs, with variability in referral patterns and steroid management, underscoring the need for education on its recognition, diagnosis, and treatment. Limited awareness regarding the use of biologic therapies in GCA and their steroid-sparing potential highlights an important educational gap. Additionally, our findings suggest that system-level interventions—such as fast-track clinics or clearer referral protocols—may support PCPs in delivering timely, coordinated care and reducing the risk of vision loss and complications of prolonged steroid use. This study was limited by a small sample size, low response rate and geographically narrow focus that may limit generalizability.

