Poster Session
Scleroderma
Poster Session C
Session: (2470–2503) Systemic Sclerosis & Related Disorders – Clinical Poster III
2487: Cardiovascular and venous thromboembolic events in systemic sclerosis: Epidemiological analysis of the Clinical Practice Research Datalink
Tuesday, October 28, 2025
10:30 AM - 12:30 PM Central Time
Location: Hall F1
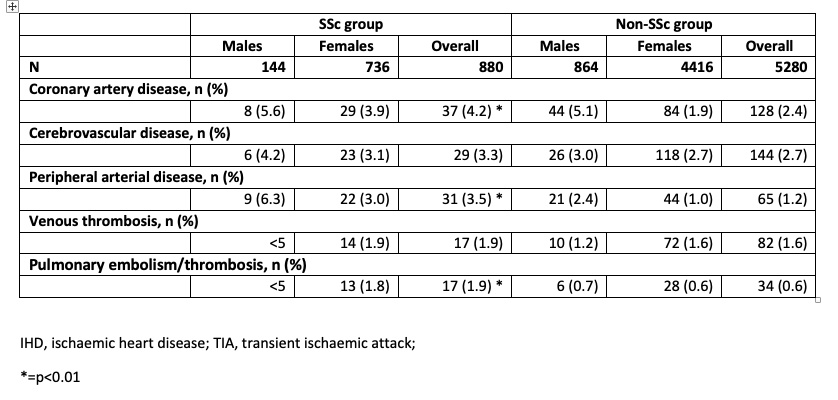
Table 1. Background proportion of subjects with cardiovascular disease and venous thromboembolism at baseline for the SSc and non-SSc groups
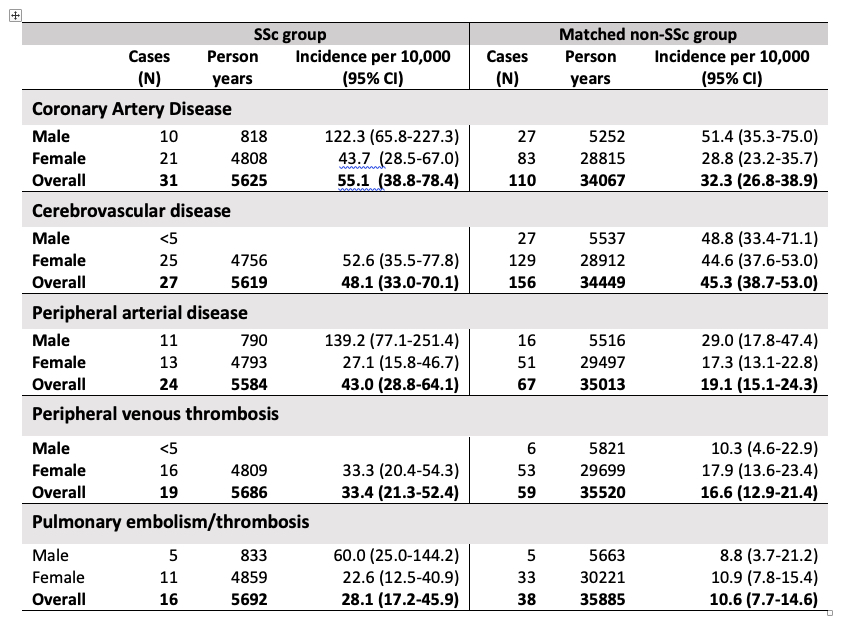
Table 2. Incidence of outcomes of cardiovascular disease for the SSc and non-SSc groups over mean of 8 years of follow up stratified for sex
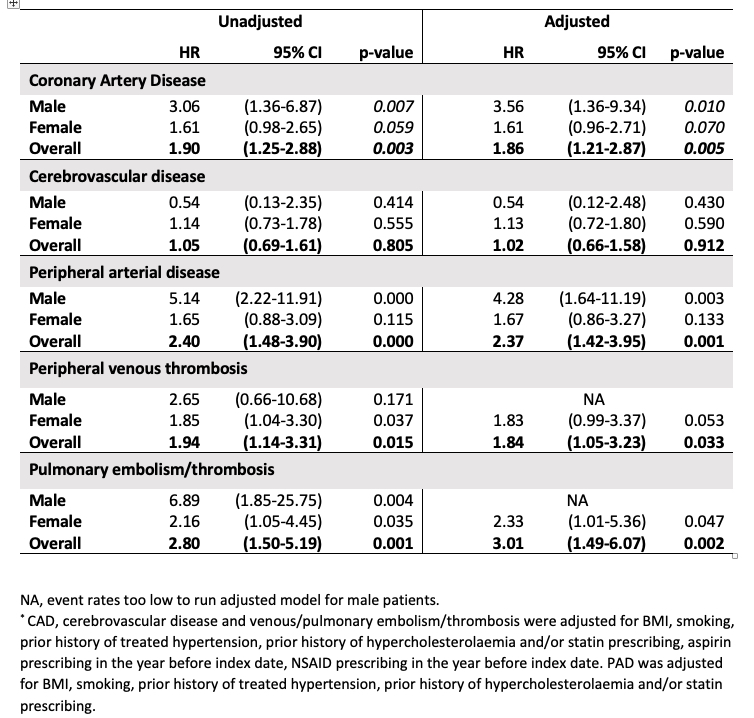
Table 3. Unadjusted and adjusted hazard ratios of cardiovascular events for SSc patients compared with non-SSc patients
.png)
John Pauling, PhD, BSc, FRCP, MBBCH
North Bristol NHS Trust & University of Bristol Medical School
Bristol, United KingdomDisclosure information not submitted.
Abstract Poster Presenter(s)
Background/Purpose: Cardiovascular disease is a leading cause of mortality in systemic sclerosis (SSc). We investigated the association between SSc and the occurrence of both cardiovascular and thromboembolic events using the Clinical Practice Research Datalink (CPRD).
Methods: A validated case-ascertainment strategy identified SSc patients in the CPRD. A cohort study design examined rates of coronary arterial disease (CAD), cerebrovascular disease, peripheral artery disease (PAD) and venous thromboembolism (VTE) in SSc patients matched to non-SSc comparators by age, sex and location in a 1:6 ratio. Prevalent and incident cases of SSc were analysed separately. Cox regression analysis was used to determine hazard ratios for event occurrence, adjusted for traditional cardiovascular risk factors.
Results: We identified 877 eligible incident cases of SSc who were matched to 5262 patients without SSc (83.7% female), with a mean follow-up of 8 years. We identified a higher background prevalence of CAD, PAD and VTE at baseline (pre-dating diagnosis) in the SSc cohort (Table 1). The incidence of CAD events in SSc males was 122.3 per 10,000 cases compared to 51.4 per 10,000 non-SSc males; whereas corresponding rates in females were lower for both groups at 43.7 and 28.8 per 10,000 in SSc and non-SSc females respectively (Table 2). Both the unadjusted and adjusted HRs for cardiovascular and VTE events are presented in Table 3. The overall adjusted HR for CAD events was 1.86 (95%CI 1.21-2.87), p=0.005. A similar but stronger association was present for PAD, with an overall adjusted HR of 2.37 (95%CI 1.42-3.95, p=0.001), which was again influenced by high incidence rates in SSc males (139.2 per 10,000 (95% CI 77.1-251.4)) compared with non-SSc male comparators (29.0 per 10,000 (95% CI 17.8-47.4)). In contrast to CAD and PAD, there was no apparent difference between the incidence of cerebrovascular disease events in SSc and non-SSc subjects, and no apparent sex-difference was observed (Tables 2 and 3). The incidence of peripheral venous thrombosis was higher than pulmonary embolism (33.4 vs. 28.1 per 10,000 SSc subjects). The risk of DVT was almost twice that found in non-SSc controls (adjusted HR: 1.84, 95%CI 1.05-3.23, p=0.033), with no sex difference in incidence rates noted. The increased risk of pulmonary thromboembolic disease was even higher with an adjusted HR of 3.01 (95%CI 1.49-6.07, p=0.002) and was increased for both sexes.
Conclusion: To our knowledge, this is the first study to demonstrate an excess risk of cardiovascular events prior to the diagnosis of SSc, in a cohort matched by age, sex and diabetes status. We have identified an increased risk of cardiovascular events and VTE, both prior to a diagnosis of SSc and within 8 years of SSc diagnosis. Work is needed to establish the mechanism of arterial/venous thrombotic events in SSc. Such insight will facilitate more targeted and effective preventative strategies and improve outcomes in SSc.

