Poster Session
Sjögren’s Disease
Poster Session B
Session: (1376–1404) Sjögren’s Disease – Basic & Clinical Science Poster II: Clinical Manifestations and Health Outcomes
1382: Interstitial lung disease in primary sjögren syndrome: pathochrony, seronegative cases, and Risk of progressive pulmonary fibrosis
Monday, October 27, 2025
10:30 AM - 12:30 PM Central Time
Location: Hall F1
- DR
Delia Reina, MD, PhD
Complex Hospitalari Universitari Moisès Broggi
Barcelona, SpainDisclosure(s): No financial relationships with ineligible companies to disclose
Abstract Poster Presenter(s)
Background/Purpose: Sjögren’s disease (SjD) is a chronic autoimmune disorder primarily targeting exocrine glands. A significant extraglandular manifestation is interstitial lung disease (ILD), which contributes to considerable morbidity and can adversely affect patient outcomes. Our aim is to describe the clinical characteristics and disease course of a primary Sjögren’s syndrome-associated ILD (pSS-ILD) cohort, with a specific focus on the proportion progressing to progressive pulmonary fibrosis (PPF).
Methods: This multicenter, retrospective, observational study included patients with pSS-ILD confirmed by high-resolution chest CT (HRCT). Diagnosis of pSS was based on anti-SSA/Ro positivity, salivary gland biopsy, or salivary gland ultrasound (grade 2 or 3 according to OMERACT SG US definitions).
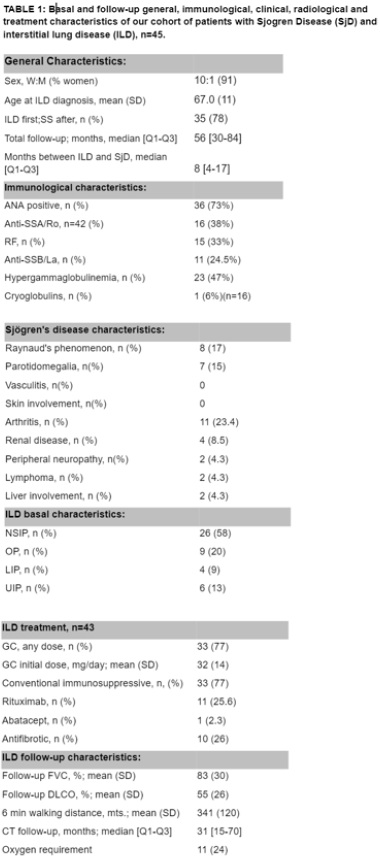
Results: A total of 45 patients (91% women) were included, with a mean age at ILD diagnosis of 67 years (SD: 11). ILD preceded pSS diagnosis in 78% (35/45), with a median lead time of 8 months (IQR: 4–17). In 22% (10/45), ILD developed after pSS, with a median interval of 48 months (IQR: 21–64.5). Anti-SSA/Ro antibodies were present in 38% (16/42), anti-SSB/La in 24.5% (11/45), and 38% (17/45) were seronegative.
Radiologically, 58% (26/45) had nonspecific interstitial pneumonia (NSIP), including 14 with fibrotic NSIP; 13% (6/45) had usual interstitial pneumonia (UIP); 20% (9/45) had organizing pneumonia (OP) or NSIP with OP; and 9% (4/45) had lymphocytic interstitial pneumonia (LIP). Follicular bronchiolitis was found in 38% (17/45).
At ILD diagnosis, mean %pFVC was 84.4 ± 21.5 (IQR: 70.8–101.7), %pDLCO was 62.2 ± 17.3 (IQR: 48–76), and 6MWT distance was 371 ± 114 m (IQR: 306–422). Mean ESSDAI was 12 (SD: 5; IQR: 7–16).
Treatment included glucocorticoids in 77% (33/43; mean prednisone dose: 32 ± 14 mg/day), immunosuppressants in 77% (mycophenolate in 31, azathioprine in 2), and biologics in 28% (rituximab in 11, abatacept in 1). Antifibrotic therapy (nintedanib or pirfenidone) was initiated in 26% (10/43) due to progression to PPF.
After a median follow-up of 56 months (IQR: 30–84), 24% (11/45) required oxygen therapy due to chronic respiratory failure, 4% (2/45) were referred for lung transplantation, and 18% (8/45) died due to ILD progression or infections.
Conclusion: ILD was the initial or predominant manifestation leading to pSS diagnosis in 78% of cases. Seronegative status was common (38%), highlighting the need to consider pSS in ILD patients with sicca symptoms. At least 26% progressed to PPF and required antifibrotic therapy.

