Poster Session
Rheumatoid Arthritis (RA)
Poster Session C
Session: (2227–2264) Rheumatoid Arthritis – Diagnosis, Manifestations, and Outcomes Poster III
2251: Dual Diagnoses, Diminished Survival: Association between rheumatoid arthritis and survival among older adults with lung cancer
Tuesday, October 28, 2025
10:30 AM - 12:30 PM Central Time
Location: Hall F1
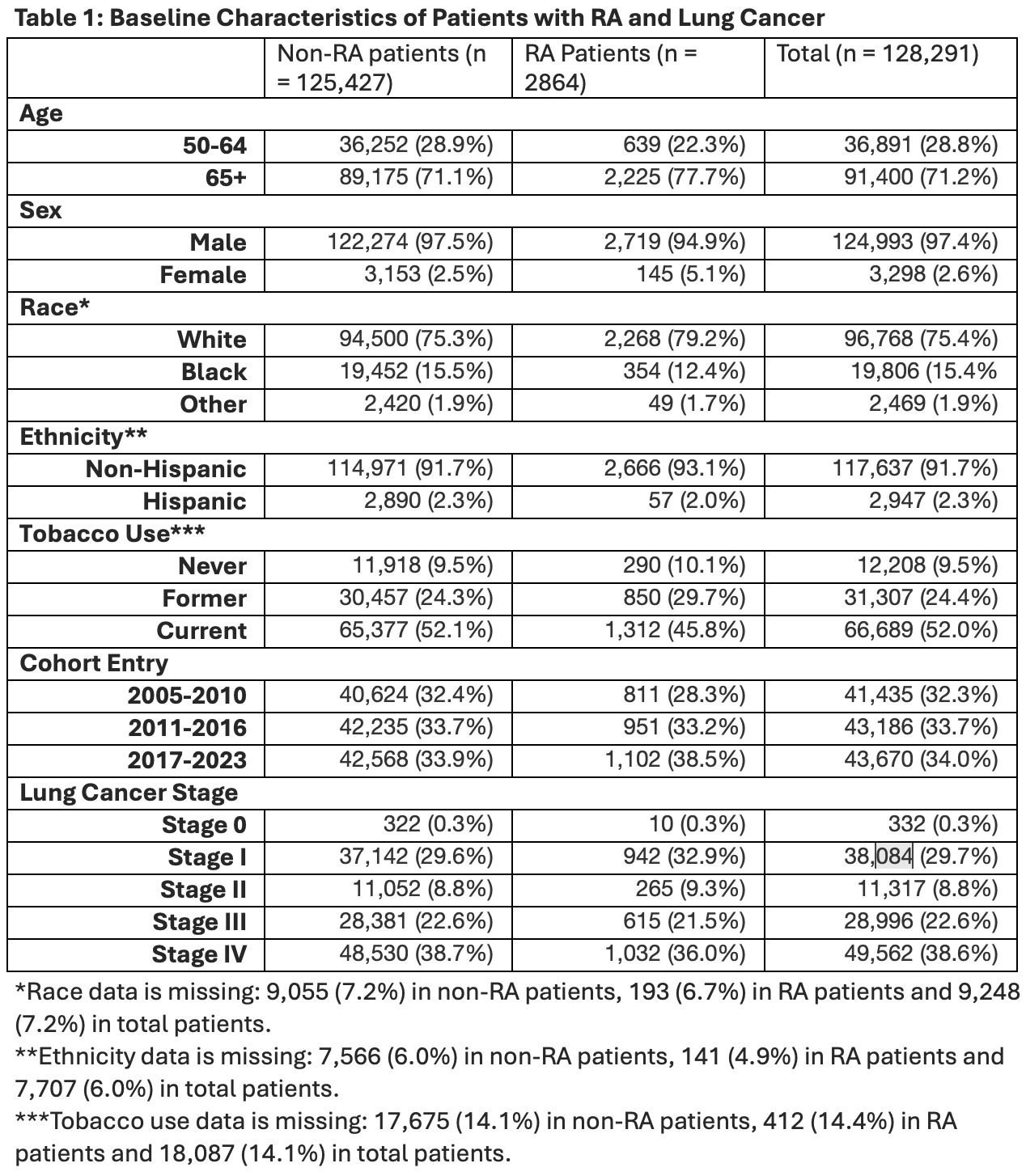
Table 1: Baseline Characteristics of Patients with RA and Lung Cancer
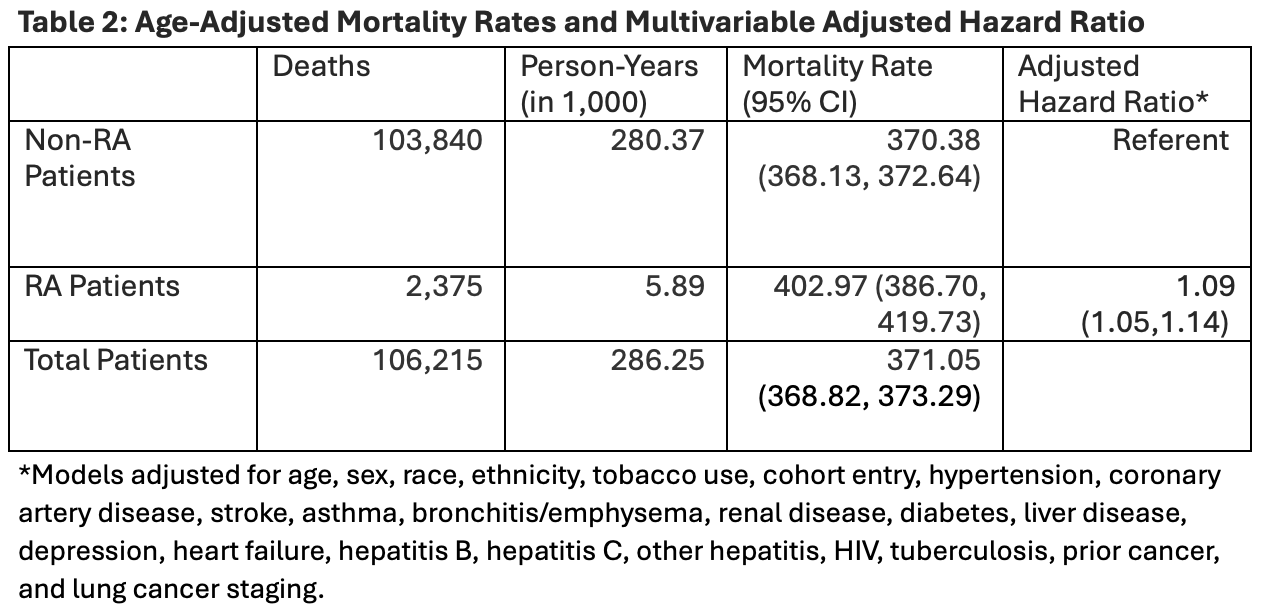
Table 2: Age-Adjusted Mortality Rates and Multivariable Adjusted Hazard Ratio
- MN
Michelle Nguyen, MD
University of Washington
Seattle, WA, United StatesDisclosure(s): No financial relationships with ineligible companies to disclose
Abstract Poster Presenter(s)
Background/Purpose: Rheumatoid arthritis (RA) is associated with an increased risk of malignancies, particularly lung cancer, relative to the general population1. However, the association between RA and overall survival in those who develop lung cancer has not been well characterized. The objective of this study was to evaluate the relationship between RA and overall survival among older adults diagnosed with lung cancer.
Methods: Data spanning 2005-2023 was obtained from the Veteran’s Health Administration’s (VHA) electronic medical records, commonly referred to as the Corporate Data Warehouse (CDW). Patients with lung cancer were identified from the Oncology Raw domain, which contains records of patients diagnosed with cancer and associated information, such as cancer stage and treatments. The cohort included patients aged 50 years or older at the time of lung cancer diagnosis. Pre-existing rheumatoid arthritis (RA) was identified based on the presence of ≥ 2 ICD-9 or ICD-10 codes for RA, 1 to 365 days apart, prior to the lung cancer diagnosis.
The association between RA and all-cause mortality was evaluated using Cox proportional hazards regression models, adjusting for demographic characteristics, smoking status, comorbid conditions, prior history of malignancy, and cancer stage at diagnosis.
Results: Among 128,291 patients with lung cancer, 2,864 (2.2%) had pre-existing RA. The cohort was predominantly male (97.4%), White (75.4%) and current smokers (52%) (Table 1). During follow-up, mortality rates were 370.4 and 403.0 per 1,000 person-years in the non-RA and RA groups, respectively. After adjusting for demographics, smoking status, comorbidities, prior malignancy, and lung cancer stage, RA was associated with increased all-cause mortality (adjusted hazard ratio 1.09; 95% CI: 1.05-1.14) (Table 2).
Conclusion: In this study using national VA data, pre-existing RA was associated with a modest but statistically significant increase in all-cause mortality. After adjusting for key clinical and demographic factors, patients with RA had a 9% higher risk of death compared to those without RA. These findings suggest that RA may independently contribute to poorer survival in patients with lung cancer, highlighting the need for integrative care strategies that address both oncologic and rheumatologic complexities in this high-risk population.

